Hypertensive Crisis: What It Is, How It Happens, and What to Do
When your blood pressure spikes suddenly and dangerously, you’re facing a hypertensive crisis, a life-threatening condition where blood pressure rises fast enough to damage organs like the heart, brain, or kidneys. Also known as a hypertensive emergency, it’s not just a high reading—it’s a medical event that can cause stroke, heart attack, or kidney failure within hours. This isn’t the same as having consistently high blood pressure. A hypertensive crisis happens when numbers shoot up past 180/120 mm Hg, often with symptoms like severe headache, blurred vision, chest pain, or trouble breathing.
What causes it? Sometimes it’s skipped medications—especially for people with long-term high blood pressure who stop taking their pills. Other times, it’s triggered by drug interactions, kidney problems, or even sudden stress. Some medications, like decongestants or illegal stimulants, can push blood pressure into crisis territory. Even skipping dialysis or having an undiagnosed adrenal tumor can be behind it. It’s not rare in people who don’t monitor their pressure or who have uncontrolled hypertension.
There’s a difference between a hypertensive emergency, where organs are already damaged and a hypertensive urgency, where pressure is sky-high but no organ damage is present yet. Both need attention, but only emergencies require hospitalization and IV drugs. Many people confuse the two and delay care—until it’s too late. If you feel dizzy, nauseous, or your head is pounding like it’s going to burst, don’t wait. Call emergency services. Waiting for symptoms to get worse is a dangerous gamble.
Most people who end up in the hospital with a hypertensive crisis were managing their blood pressure poorly for months or years. They might’ve thought their meds were working fine, or they stopped because of side effects like dizziness or fatigue. Others didn’t even know they had high blood pressure until the crisis hit. The truth? High blood pressure often has no warning signs—until it does, and then it’s too late.
What happens next? Doctors use fast-acting drugs to bring pressure down—slowly. Too fast, and you risk stroke or organ damage from sudden drops. Common treatments include IV labetalol, nitroprusside, or oral nifedipine. But the real fix? Long-term management. That means consistent meds, regular checkups, and lifestyle changes. Cutting salt, losing weight, and avoiding alcohol aren’t optional—they’re part of survival.
What you’ll find in the posts below isn’t just theory. You’ll see real stories and data on how common medications interact with blood pressure, what to avoid when you’re at risk, and how to spot trouble before it becomes a crisis. From how heat affects blood pressure meds to how dehydration can trigger dangerous spikes, these posts give you the tools to act—not just react. This isn’t about guessing. It’s about knowing what to look for, what to ask your doctor, and how to stay out of the ER.
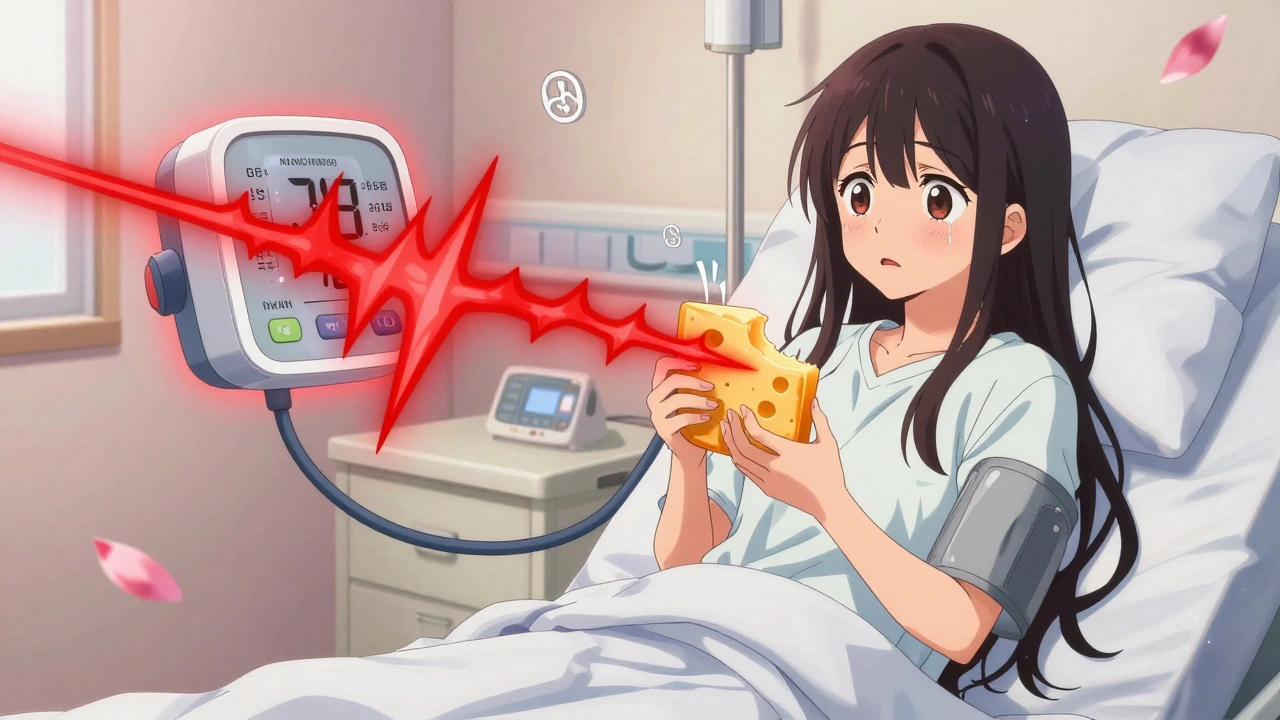
Severe Hypertensive Crisis from Drug Interactions: What You Need to Know
A severe hypertensive crisis can be triggered by common drug interactions-like antidepressants with cold medicine or cheese with MAOIs. Learn the signs, risks, and how to prevent a life-threatening emergency.

MAO Inhibitors: Dangerous Interactions with Common Medications
MAO inhibitors can save lives-but they can also cause deadly reactions when mixed with common medications, supplements, or foods. Know the risks of serotonin syndrome and hypertensive crisis before taking one.
-
14.11.25 -
Alistair Mukondiwa -
9
- Drug Information (69)
- Health and Wellness (59)
- Pharmacy Information (23)
- Medical Conditions (22)
- Supplements (4)
- Diabetes (4)
- Travel Health (3)
- Mental Health (3)
- Heart Health (2)
- Parenting (2)
-
Severe Hypertensive Crisis from Drug Interactions: What You Need to Know
12 Dec 2025 -
Obesity Pathophysiology: How Appetite and Metabolism Go Wrong
1 Dec 2025 -
Statins and ALS: What the Latest Science Really Says
23 Nov 2025 -
AI and Pharmacogenomics: How Personalized Generic Recommendations Are Changing Online Pharmacies
15 Dec 2025 -
Buy Generic Tamoxifen Online in Australia: Safe, Legal, and Low-Cost Options (2025)
9 Sep 2025

12.12.25
Alistair Mukondiwa
13