Drug Interaction Risk Checker for Hypertensive Crisis
Check if your medications could trigger a severe hypertensive crisis. This tool identifies dangerous combinations based on the latest medical guidelines. Note: This is for informational purposes only and does not replace professional medical advice.
Type medication name and press Add. Click to remove any medication.
Risk Assessment
When your blood pressure spikes suddenly to 220 over 130, it’s not just a bad day-it’s a life-threatening emergency. This is a severe hypertensive crisis, and in many cases, it’s not caused by years of poor diet or genetics. It’s caused by something you took-maybe a common cold medicine, an antidepressant, or even a piece of aged cheese. These reactions don’t always show up on a doctor’s radar, but they’re more common than you think-and they’re often preventable.
What Exactly Is a Hypertensive Crisis?
A hypertensive crisis happens when your blood pressure shoots past 180/120 mmHg. That’s not just high-it’s dangerous. At this level, the force of blood rushing through your arteries can tear blood vessels, damage your kidneys, cause a stroke, or trigger heart failure. There are two types: urgency and emergency. Urgency means your pressure is sky-high but your organs aren’t damaged yet. Emergency means your organs are already under attack. The difference? Minutes matter.Drugs That Can Trigger a Crisis
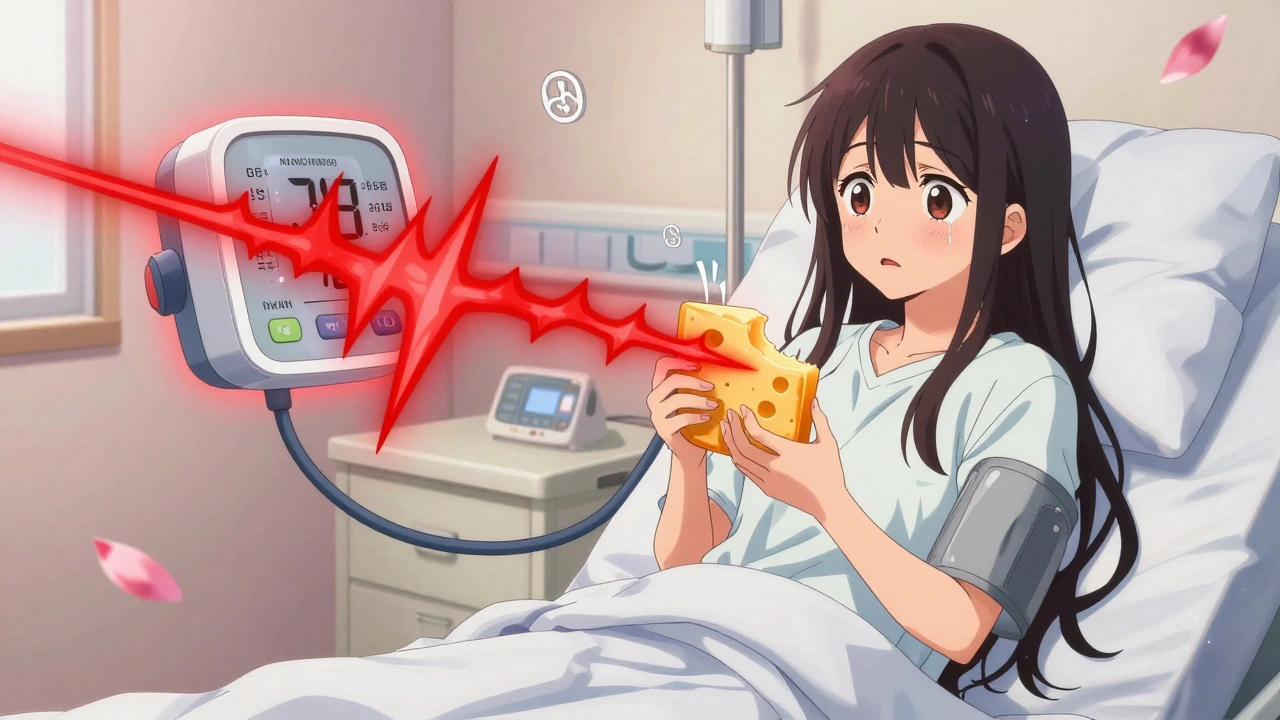
Most people assume high blood pressure comes from salt, stress, or being overweight. But up to 20% of severe cases are caused by drugs-either alone or in combination. Some of the most dangerous offenders include:- MAO inhibitors (MAOIs) like phenelzine or selegiline, used for depression or Parkinson’s. These drugs block the breakdown of neurotransmitters. If you eat tyramine-rich foods-aged cheese, cured meats, tap beer-you get a massive surge of norepinephrine. Blood pressure can spike over 250 mmHg in under an hour.
- Venlafaxine (Effexor), especially at doses above 300 mg/day. This antidepressant increases norepinephrine and serotonin. At high doses, it can push diastolic pressure above 90 mmHg. Many patients report headaches and blurred vision, but doctors often dismiss it as "anxiety symptoms."
- Cocaine combined with beta-blockers like propranolol. Cocaine causes vasoconstriction. Propranolol blocks the heart’s response but leaves blood vessels wide open to unopposed stimulation. The result? Systolic pressure over 220 mmHg.
- Cyclosporine, used after organ transplants. It affects kidney function and sodium balance. Up to half of transplant patients on this drug develop hypertension so severe they need multiple medications just to control it.
- Decongestants like pseudoephedrine. Found in cold and allergy meds, they’re harmless for most-but deadly when mixed with antidepressants or in people with undiagnosed high blood pressure.
- Licorice candy. Yes, candy. The glycyrrhizin in licorice mimics aldosterone, causing your body to retain salt and lose potassium. People who eat a few pieces daily for weeks can develop low potassium, swelling, and blood pressure over 190/110.
Why These Reactions Are So Dangerous
It’s not just the number on the monitor. It’s what happens inside your body. When pressure spikes, tiny blood vessels in your brain, kidneys, and eyes start to leak. Fluid builds up. Cells die. In the brain, this can cause a hemorrhagic stroke. In the kidneys, it can lead to acute failure. In the heart, it can trigger a heart attack-even in someone with no prior history. The worst part? Many of these reactions are invisible until it’s too late. A 2021 study found that 68% of patients who had a drug-induced crisis had complained of "unexplained headaches" or "blurred vision" to their doctors months before. But only 22% had their medications reviewed. Doctors often assume the symptoms are stress, migraines, or aging-not a deadly interaction.
Real Stories Behind the Numbers
One Reddit user, u/MigraineWarrior, wrote: "I ate a slice of cheddar with my selegiline. Woke up with a splitting headache. BP was 220/130. Three days in ICU. Still scared to eat cheese." He wasn’t told the risk. His doctor didn’t ask about his diet. The interaction was never flagged. Another patient, on venlafaxine, noticed her blood pressure creeping up over months. Her doctor told her to "drink less coffee." She kept taking the medication. At 400 mg/day, her diastolic hit 110. She ended up in the ER with kidney damage. Her prescription had no warning. And then there’s the licorice case documented in a 2022 journal. A 62-year-old woman had persistent high blood pressure despite taking three medications. Her cardiologist couldn’t figure it out. Then she mentioned she ate a small bag of black licorice candy every day. After stopping it, her BP dropped to normal in two weeks. No new meds. No surgery. Just a candy bar.What You Should Do If You’re on High-Risk Medications
If you’re taking any of these drugs, here’s what you need to know:- Know your meds. Write down every pill, supplement, and OTC product you take-including herbal teas and cough syrups.
- Ask about interactions. Don’t assume your doctor knows. Say: "Could any of these medications raise my blood pressure?" Especially if you’re on antidepressants, immunosuppressants, or stimulants.
- Watch for red flags. Sudden headaches, chest tightness, blurred vision, nosebleeds, or swelling in your legs could be early signs. Don’t wait for a "hypertensive crisis" to happen.
- Check your diet. If you’re on an MAOI, avoid aged cheeses, cured meats, soy sauce, fermented foods, and tap beer. Use apps like "MAOI Diet Helper"-a 2021 Mayo Clinic study showed it improved adherence by 78%.
- Monitor your BP. Buy a home monitor. Check it weekly if you’re on venlafaxine or cyclosporine. If you’re on an MAOI, check it daily for the first month.
How Doctors Are Starting to Catch These Cases
The medical system is slowly waking up. In 2023, the FDA approved the first AI-powered tool that scans electronic health records for dangerous drug combinations. In trials, it cut MAOI-related emergencies by 40%. Hospitals are now training staff to ask three questions when someone shows up with high BP: "What are you taking?" "When did you start?" "Did you change anything recently?" The American College of Cardiology updated its 2024 guidelines to classify venlafaxine doses above 225 mg/day as "high risk," requiring quarterly BP checks. Genetic testing for CYP2D6 enzyme variations is now being offered to patients on certain antidepressants-those with slow metabolism are 3.2 times more likely to have a severe reaction.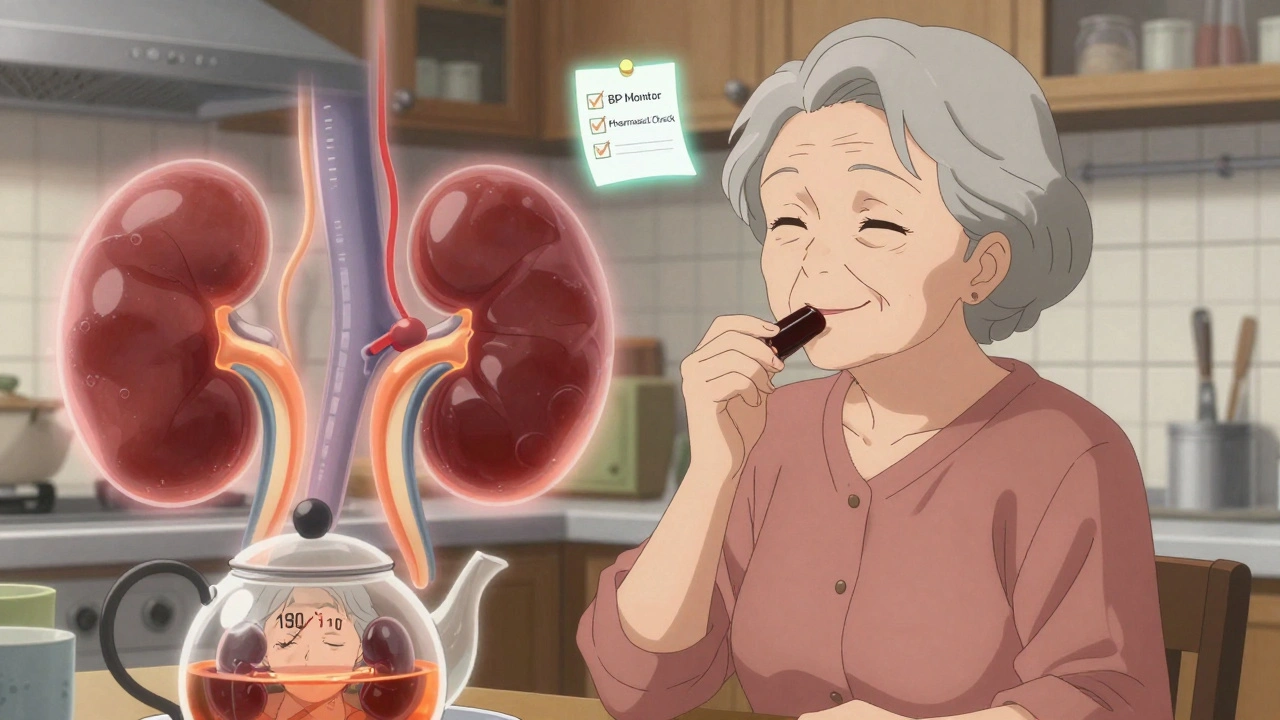
What’s Still Not Being Done
Despite all this, the system is still failing. A 2022 JAMA study found that 78% of high-risk medications don’t have clear warnings about hypertensive crisis on their labels. Over-the-counter decongestants? Only 12% have adequate warnings. Most patients don’t know that NyQuil or Sudafed can be deadly with their antidepressants. And in older adults on five or more medications-common in Australia, the US, and Europe-the risk is rising fast. By 2027, experts predict a 35% increase in drug-induced crises, mostly from weight-loss pills and antidepressants.What to Do in an Emergency
If your blood pressure is above 180/120 and you have symptoms like chest pain, confusion, or difficulty breathing: call emergency services immediately. Do not wait. Do not take extra pills. Do not try to "relax it down." In the ER, doctors will use specific drugs based on the cause:- For MAOI-tyramine reactions: IV phentolamine (92% effective within 20 minutes)
- For MAOI or stimulant-induced: Labetalol (85% effective)
- For cyclosporine-related: Calcium channel blockers like amlodipine (78% effective)
Prevention Is the Only Real Cure
You don’t need to avoid all medications. But you do need to be informed. A severe hypertensive crisis from a drug interaction isn’t bad luck-it’s a system failure. And it’s preventable. If you’re on antidepressants, immunosuppressants, or stimulants, talk to your pharmacist. Ask for a full interaction check. Bring a list of everything you take-including vitamins and herbal supplements. If your doctor brushes you off, get a second opinion. Your blood pressure isn’t just a number. It’s a warning sign. And sometimes, the warning comes from something you thought was harmless.Can over-the-counter cold medicine cause a hypertensive crisis?
Yes. Decongestants like pseudoephedrine and phenylephrine can cause dangerous spikes in blood pressure, especially when taken with antidepressants like SSRIs or MAOIs. Even a single dose can trigger a crisis in someone with undiagnosed hypertension. Always check with a pharmacist before taking OTC meds if you’re on any prescription drugs.
Is it safe to eat cheese while on an MAOI?
No. Aged cheeses like cheddar, parmesan, and blue cheese contain high levels of tyramine, which can cause a sudden, life-threatening rise in blood pressure when combined with MAOIs. Even small amounts can trigger a crisis. Some newer MAOIs like selegiline patches have lower risk, but you should still avoid tyramine-rich foods unless your doctor confirms it’s safe.
How long does it take for a drug-induced hypertensive crisis to resolve?
It depends on the drug. Cocaine or MAOI reactions can stabilize within hours after stopping the substance and receiving treatment. But mineralocorticoid-related crises-like those from licorice or corticosteroids-can last weeks because the body’s hormone balance takes time to reset. Blood pressure may remain high for 10-14 days after stopping licorice, even with medication.
Can I stop my antidepressant if my blood pressure rises?
Never stop abruptly. Stopping antidepressants like venlafaxine suddenly can cause withdrawal symptoms, including rebound high blood pressure. If you notice rising BP, contact your doctor. They may lower your dose, switch medications, or add a blood pressure drug. Always manage changes under medical supervision.
Are there any safe alternatives to venlafaxine if it raises my blood pressure?
Yes. Bupropion (Wellbutrin) and sertraline (Zoloft) are less likely to raise blood pressure and are often used as alternatives. However, bupropion can still increase BP in high doses, so monitoring is still needed. Your doctor can use genetic testing (CYP2D6) to help choose the safest option based on how your body metabolizes drugs.
Why don’t doctors always check for drug interactions?
Many doctors don’t have time to review every medication during a short appointment. Electronic health records often don’t flag interactions unless they’re severe or FDA-recognized. A 2015 study found 65% of emergency doctors never checked for drug interactions in hypertensive crisis cases. Patients need to be their own advocates-bring a full list of everything you take, including supplements and OTC drugs.
Can I use home blood pressure monitors to prevent a crisis?
Absolutely. Home monitoring is one of the most effective prevention tools. If you’re on high-risk meds like venlafaxine, cyclosporine, or MAOIs, check your BP at least twice a week. Record the numbers and bring them to your appointments. A consistent rise of 10-15 mmHg over a few weeks is a red flag-even if you feel fine.
If you’re on multiple medications, especially for chronic conditions, your risk of a drug-induced hypertensive crisis is higher than you think. But awareness, communication, and simple monitoring can save your life. Don’t wait for a crisis to happen. Ask the questions now.

This is such an important post. I'm a nurse, and I've seen too many patients come in with BP over 200/120 because they took Sudafed with their antidepressant and thought it was 'just a headache.' The lack of clear warnings on OTC meds is terrifying. Please, if you're on MAOIs or venlafaxine-ask your pharmacist before taking anything new. Even ibuprofen can interact in some cases. You're not overreacting-you're being smart.
And yes, licorice candy is a real culprit. I had a patient who ate a bag a week for months. Her BP dropped 40 points in two weeks after she stopped. No meds changed. Just candy. Mind blown.
Share this. Someone you love might need it.
OMG I just realized I’ve been eating black licorice every day for my ‘energy boost’ 😱 I’m so sorry, my kidneys… I’m throwing out my candy drawer rn 🙈💖 #lifelesson #bpawareness
Thank you for writing this with such clarity. I’ve been on selegiline for Parkinson’s for 5 years, and no one ever told me about the cheese thing. I ate blue cheese on a charcuterie board last Christmas. I thought my headache was from wine. I’m lucky I didn’t end up in the ICU. This should be mandatory reading for every patient on antidepressants or MAOIs. Please, doctors-don’t assume we know. We don’t.
Also, the MAOI Diet Helper app? Saved my life. I use it every time I go grocery shopping now.
One must question the methodology behind these claims. The data presented lacks proper peer-reviewed citations for the 68% statistic regarding unexplained headaches. Moreover, the assertion that licorice candy can induce hypertensive crisis is anecdotally overstated. The glycyrrhizin content in commercial confectionery is typically below toxic thresholds. One suspects this article was written to generate alarm rather than inform. The FDA has not issued any such warnings regarding licorice in the context of hypertension. One must remain skeptical of sensationalized medical narratives.
Wow. So let me get this straight: eating cheese, taking NyQuil, and having a sweet tooth could kill me… but my doctor says ‘just drink less coffee’? 🙄 I’m not mad… I’m just disappointed. And also terrified. I’m printing this out and taping it to my fridge. And my doctor’s door. And my therapist’s waiting room. Just in case.
lol this is just Big Pharma gaslighting you. They don’t want you to know that the real cause of hypertension is 5G radiation + fluoride in the water. But hey, go ahead and blame cheese and candy. Meanwhile, the FDA is busy hiding the truth about how your meds are actually making you sick. 🤡
PS: My cousin’s neighbor’s dog got BP spikes after eating a bag of Skittles. Coincidence? I think not.
This is a textbook case of medical overreach. You’re telling people to avoid cheese because of a drug they’re taking? That’s not medicine-that’s fearmongering. If you’re on an MAOI, you should be monitored, not infantilized. And why are we suddenly treating patients like children who can’t handle basic nutrition? This isn’t prevention-it’s control. I’ve been on cyclosporine for 12 years. My BP is fine. My diet is fine. Stop scaring people with cherry-picked anecdotes.
As a pharmacist, I see this ALL THE TIME. Patients come in with BP 210/130, and they’re like, ‘I just took DayQuil for my cold.’ I ask, ‘Are you on an antidepressant?’ They say, ‘Yeah, but my doctor said it was fine.’
Here’s the thing: drug interactions aren’t always in the EHR. Sometimes the system doesn’t flag it. That’s why you need to speak up. Bring your list. Ask: ‘Could this combo raise my BP?’
And yes-licorice candy is real. I had a guy who ate 3 bags a week. His potassium was 2.8. He didn’t even know it was in candy. 😳
Stay safe. Stay informed. You’re your best advocate.
This is a critical piece of public health information that deserves far more attention. The medical community has long underestimated the role of polypharmacy and dietary interactions in acute hypertensive events. While the examples cited are compelling, I would encourage readers to also consider the broader systemic issue: the fragmentation of care. Patients on multiple specialists often have no single provider reviewing all medications holistically.
Furthermore, the emergence of AI-driven interaction screening tools, as mentioned, represents a significant step forward-but adoption remains uneven. Until these systems are universally integrated and mandated, patient education and proactive communication remain the most reliable defenses.
Thank you for highlighting the human stories behind the statistics. They are the reason we must do better.
As someone who’s been on venlafaxine for 7 years, I just want to say: I didn’t know any of this until I read this post. My BP was creeping up, and I thought it was stress. I started checking it at home, and sure enough-over 140/90 every morning. I talked to my doctor, we lowered my dose, and switched me to sertraline. My BP’s been normal for 6 months now.
You’re not crazy if you feel off. You’re not ‘anxious.’ You’re having a reaction. Listen to your body. And if your doctor doesn’t listen? Find a new one. You deserve better.
Y’all this is wild but also so real. I had no idea licorice candy was a thing 😭 I thought it was just sugar! I’ve been eating it since I was a kid. My mom’s got hypertension and she eats it daily. I’m gonna text her RIGHT NOW. Also, I bought a home BP monitor today. First time I’ve ever done it. I feel like a responsible adult now 🥲💪 #healthwin
Okay but what if… the whole thing is a lie? 🤔 What if the FDA, Big Pharma, and your doctor are all in on it? What if the ‘hypertensive crisis’ is just a way to sell you more meds? I read this and I thought: why do they always blame the patient’s diet or OTC meds? Why not the pills they’re prescribing? Why not the toxins in our water? Why not the EMFs? I’m not saying it’s false-I’m saying it’s incomplete. There’s a bigger picture. And they don’t want you to see it. 🕵️♀️👁️🗨️
So let me get this straight: I can’t have a cold medicine, cheese, or candy without risking death? And my doctor’s too lazy to check interactions? This is why America’s healthcare is broken. I’m not even on any of these meds-I’m just a guy who likes a good snack-and now I’m scared to live. I’m moving to Canada. At least they don’t poison us with licorice here. 🇨🇦 #freedom