MAO inhibitors aren’t just another antidepressant. They’re a high-stakes medication that can turn a simple cold medicine or a slice of aged cheese into a medical emergency. If you’re taking one-whether it’s phenelzine, tranylcypromine, or the selegiline patch-you need to know what not to mix it with. Because the risks aren’t theoretical. They’re life-or-death.
What Are MAO Inhibitors?
MAO inhibitors, or MAOIs, are a class of antidepressants that work by blocking the enzyme monoamine oxidase. This enzyme normally breaks down neurotransmitters like serotonin, norepinephrine, and dopamine. When it’s turned off, these chemicals build up in the brain, which can lift mood in people with treatment-resistant depression or atypical depression. The first MAOI, iproniazid, was discovered in the 1950s by accident-researchers were studying tuberculosis when they noticed patients felt unusually happy.
Today, MAOIs are rarely the first choice. They’re mostly used when other antidepressants like SSRIs have failed. Less than 1% of all antidepressant prescriptions in the U.S. are for MAOIs. But that small number still adds up to thousands of people who rely on them-and who need to avoid dangerous combinations.
The Two Biggest Dangers: Hypertensive Crisis and Serotonin Syndrome
There are two major dangers with MAOIs. One is a sudden, dangerous spike in blood pressure called a hypertensive crisis. The other is serotonin syndrome-a potentially fatal overload of serotonin in the nervous system.
Hypertensive crisis happens when tyramine-a compound found in certain foods and drinks-builds up in your body. Normally, monoamine oxidase breaks down tyramine. But if you’re on an MAOI, that doesn’t happen. Tyramine then triggers a massive release of norepinephrine, which can send your blood pressure soaring. Systolic pressure can jump 60 to 100 mmHg in under two hours. In extreme cases, it hits 250 mmHg. That’s enough to cause stroke, heart attack, or death.
Serotonin syndrome occurs when MAOIs are combined with other drugs that increase serotonin. This isn’t just about feeling a little jittery. Symptoms range from shivering and diarrhea to seizures, high fever (over 41°C), muscle breakdown, and organ failure. About 2-12% of severe cases are fatal. It can happen within hours of taking a new medication.
Medications That Can Kill You When Mixed With MAOIs
Some of the most common drugs you might take-without even realizing it-are deadly with MAOIs.
- Dextromethorphan - Found in over 100 cough syrups and cold medicines. A single 30mg dose combined with phenelzine has triggered hospitalization. The FDA issued a warning in 1992. Many products still don’t have clear warnings.
- SSRIs and SNRIs - Fluoxetine (Prozac), sertraline (Zoloft), venlafaxine (Effexor). Mixing these with MAOIs can cause serotonin syndrome. You need a 14-day gap between stopping one and starting the other. For fluoxetine, wait five weeks because it sticks around in your system so long.
- Tramadol, meperidine, methadone - These opioids are absolute no-gos. A 32-year-old man was intubated after taking tramadol while on selegiline. He didn’t even know it was dangerous.
- Linezolid - An antibiotic used for tough infections. It’s also an MAOI. Combining it with an oral MAOI led to a fatal case in 2008. Doctors now avoid this combo entirely.
- Phenylephrine - A common decongestant in cold and allergy meds. It directly raises blood pressure. With an MAOI, it’s a recipe for hypertensive crisis.
- Ephedrine - Even though ephedra was banned in 2004, some supplements still contain it. It’s extremely dangerous with MAOIs. Emergency room visits have been documented within 30 minutes of use.
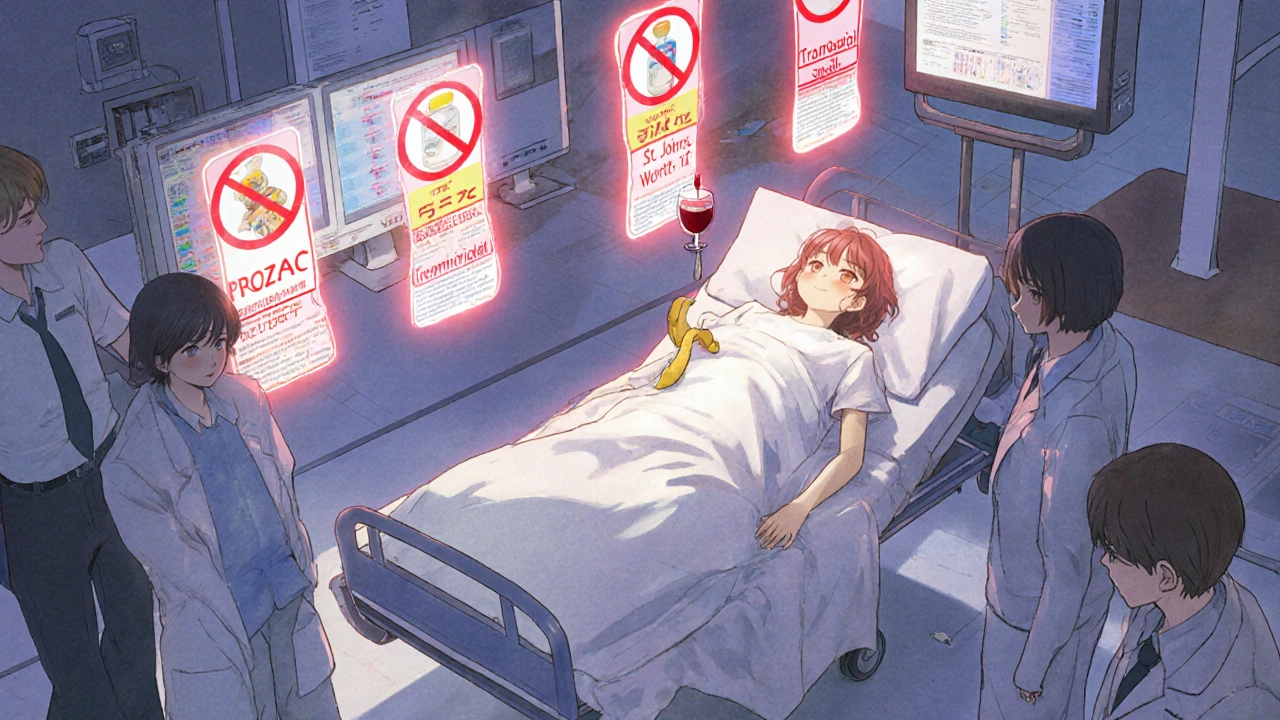
Supplements and Herbal Products to Avoid
You might think herbal means safe. Not with MAOIs.
- St. John’s Wort - A popular natural antidepressant. It increases serotonin. Combined with an MAOI, it’s caused severe serotonin syndrome, including fever over 40°C and blood pressure above 220/110.
- 5-HTP - Sold as a sleep or mood aid. It’s a direct precursor to serotonin. One case report showed a patient on phenelzine developed life-threatening symptoms after taking just 200mg.
- SAMe (S-adenosylmethionine) - Used for joint pain and depression. It also boosts serotonin. The American Psychiatric Association explicitly warns against it with MAOIs.
- Ginseng - A 1985 case linked ginseng to mania and tremors in someone on phenelzine. Some researchers suspect caffeine contamination, but the risk is real enough to avoid it.
Dietary Triggers: What You Can’t Eat
It’s not just pills. Your lunch could be dangerous.
MAOIs block the enzyme that breaks down tyramine. That means foods high in tyramine can cause a spike in blood pressure. The threshold for danger is around 10-25mg. A single ounce of aged cheese can contain 15mg.
- Aged cheeses - Cheddar, blue cheese, Swiss, parmesan. Avoid anything aged more than six months.
- Cured and fermented meats - Pepperoni, salami, sausage, pickled herring.
- Fermented soy - Soy sauce, miso, tempeh.
- Tap and draft beer - Contains 8-20mg tyramine per 12oz. Bottled beer is usually safe.
- Red wine - Especially Chianti and other aged varieties. White wine is lower risk.
- Overripe fruits - Bananas, avocados, figs. Eat them fresh, not mushy.
There’s one exception: the selegiline patch (Emsam) at the lowest dose (6mg/24hr). Studies show it doesn’t interact with tyramine at this level. You can eat normally. But if you increase the dose, the restrictions come back.
What About Switching Medications?
If you’re switching from an MAOI to an SSRI-or vice versa-you can’t just stop one and start the other the next day.
Doctors require a washout period. For most MAOIs, it’s 14 days. For fluoxetine, it’s five weeks. Why? Because fluoxetine and its active metabolite, norfluoxetine, stay in your body for weeks. If you start an SSRI too soon, you’re asking for serotonin syndrome.
Electronic health records now block prescriptions that mix MAOIs with contraindicated drugs. This started after 19 fatal interactions were reported between 1998 and 2003. But mistakes still happen. A 2021 study found 34% of primary care doctors didn’t know dextromethorphan was dangerous with MAOIs.

What Should You Do?
If you’re on an MAOI:
- Carry a wallet card listing all contraindicated drugs. About 78% of psychiatrists give these to patients.
- Always check with your pharmacist before taking any new medication-prescription, OTC, or herbal.
- Read labels on cold, cough, and sleep meds. Look for dextromethorphan, phenylephrine, or pseudoephedrine.
- Don’t assume “natural” is safe. St. John’s Wort and 5-HTP are not harmless.
- If you feel sudden headache, chest pain, confusion, high fever, or muscle stiffness-seek emergency help immediately.
MAOIs are powerful tools. But they demand respect. One wrong pill, one bite of blue cheese, one missed warning label-and you could be in serious danger.
Why Are MAOIs Still Used?
Because for some people, they work when nothing else does. People with treatment-resistant depression, atypical depression (with oversleeping, overeating, mood reactivity), or severe anxiety disorders often find relief with MAOIs. The transdermal patch version (selegiline) has made them safer and easier to use. Today, 68% of MAOI prescriptions are for the patch, not pills.
But they’re not for everyone. They’re for people who’ve tried everything else-and who are willing to follow strict rules. If you’re considering an MAOI, make sure your doctor is experienced with them. And if you’re already on one, don’t take chances.
Can I take Tylenol (acetaminophen) with MAOIs?
Yes, acetaminophen (Tylenol) is safe to take with MAOIs. It doesn’t affect serotonin or norepinephrine levels. It’s one of the few pain relievers you can use without risk. Avoid NSAIDs like ibuprofen or naproxen if you have high blood pressure, but acetaminophen is generally fine.
Is caffeine dangerous with MAOIs?
Caffeine isn’t directly dangerous with MAOIs, but it can worsen side effects like jitteriness, rapid heartbeat, or high blood pressure. If you’re prone to anxiety or hypertension, limit coffee, energy drinks, and strong tea. A couple of cups a day are usually okay, but monitor how you feel.
What if I accidentally take a contraindicated drug?
Call emergency services or go to the nearest ER immediately. Don’t wait for symptoms. If you took dextromethorphan, phenylephrine, or an SSRI within the last 24 hours, tell them you’re on an MAOI. Early treatment with benzodiazepines and cooling measures can be lifesaving.
Can I drink alcohol while on MAOIs?
Avoid alcohol. It can cause a sudden spike in blood pressure and increase drowsiness or dizziness. Some wines and beers also contain tyramine. Even if your MAOI is the patch, alcohol adds unnecessary risk. Stick to non-alcoholic drinks.
Are MAOIs safe during pregnancy?
There’s limited data, but MAOIs are generally not recommended during pregnancy. They cross the placenta, and risks to the fetus aren’t fully understood. If you’re pregnant or planning to be, talk to your psychiatrist about safer alternatives. Never stop an MAOI suddenly without medical supervision.
Final Thought: Know Your Meds
MAOIs are not outdated-they’re just misunderstood. They work. But they demand attention. The danger isn’t in the drug itself. It’s in the silence around it. A patient takes a cold medicine because they feel sick. A doctor prescribes an antibiotic without knowing the patient’s full history. A friend recommends St. John’s Wort. And suddenly, it’s too late.
If you’re on an MAOI, you’re part of a small but critical group. Your safety depends on knowing what to avoid-and speaking up when others don’t. Keep your list of dangerous drugs handy. Talk to your pharmacist every time you get a new prescription. And never assume something is safe just because it’s over the counter.


OMG I had no idea aged cheese could kill you?? 😱 I just ate a slice of cheddar with my wine last night… I’m gonna check my meds right now. Thanks for the wake-up call!!
MAOIs represent a profound paradox in modern psychiatry: they are among the most effective tools for treatment-resistant depression, yet they are shrouded in fear due to preventable, often poorly communicated risks. The real failure is not the drug-it’s the system that fails to educate patients, pharmacists, and primary care providers with the same rigor as it does for anticoagulants or insulin. This isn't just about avoiding tyramine-it's about institutional accountability.
why do we even still use these old ass drugs?? like who even eats blue cheese anymore? i bet 90% of people on these are just dumb and forgot to read the label. also why is the FDA so slow??
MAOI pharmacokinetics demand strict adherence to monoamine homeostasis protocols. Tyramine ingestion bypasses enzymatic degradation, triggering catecholamine surge via adrenergic receptor agonism. Dextromethorphan’s NMDA antagonism + SERT inhibition creates synergistic serotonergic toxicity. Clinical vigilance is non-negotiable.
USA still uses these 1950s relics? In India we’ve moved to precision psychiatry with genetic testing and SSRIs. This is why your healthcare system is broken-still letting people die because doctors don’t update their knowledge. Also, who eats fermented soy? That’s just weird.
Let me be clear: this isn’t about medication-it’s about personal responsibility. You want to live? Then you must become the architect of your own survival. The world doesn’t owe you safety. You must memorize every contraindication. Every label. Every warning. If you forget? Then you deserve what happens. No one else is responsible for your ignorance. And yes-I’ve seen it happen. People die because they thought ‘natural’ meant ‘safe.’ They’re wrong.
There’s something haunting about how these drugs operate in the shadows-so potent, so lethal, yet so quietly prescribed. We treat them like relics, but they’re not. They’re the last resort for those who’ve been abandoned by every other option. The tragedy isn’t the interaction-it’s the silence that precedes it. Who speaks up when the patient doesn’t know to ask?
Acetaminophen is safe. Caffeine is fine in moderation. Alcohol? Skip it. Always check with your pharmacist. Carry your list. This info saves lives. Thank you for writing this clearly.
Look I’ve been on selegiline patch for 3 years and I eat blue cheese and drink red wine and I’m fine. Everyone’s just scared of the word MAOI. You don’t need to live like a monk. The patch is safe. The warnings are outdated. I’ve seen more people hurt by anxiety over this than by the actual drug. Chill out. Your brain needs this. Don’t let fear steal your life.