When you have lupus, your immune system doesn’t just attack foreign invaders-it turns on your own body. For about 9 out of 10 people with systemic lupus erythematosus (SLE), that means painful, swollen joints. This isn’t the same as osteoarthritis or even typical rheumatoid arthritis. Lupus arthritis hits the small joints in your hands, wrists, and knees, often symmetrically, and while it’s painful and stiff, it rarely causes permanent bone damage. But the constant ache, the morning stiffness that lasts for hours, the swelling that comes and goes-it wears you down. And that’s where hydroxychloroquine, sold under the brand name Plaquenil, steps in.
Why Hydroxychloroquine Is the First-Line Treatment for Lupus Arthritis
Hydroxychloroquine isn’t new. It was originally developed in the 1940s as an antimalarial drug. But in the 1950s, doctors noticed something strange: patients with lupus or rheumatoid arthritis who took it for malaria felt better. Their joints hurt less. Their skin rashes faded. Their fatigue improved. Decades later, it’s still the most widely prescribed medication for lupus arthritis-and for good reason.
According to the European League Against Rheumatism (EULAR) and the American College of Rheumatology, hydroxychloroquine is recommended for every person diagnosed with SLE, no matter how mild their symptoms. That’s a Grade A recommendation, based on evidence from over 95 studies. Why? Because it doesn’t just treat joint pain-it changes the course of the disease.
Studies show that people taking hydroxychloroquine have at least a 50% lower chance of having a major lupus flare. That means fewer hospital visits, fewer steroid bursts, and less risk of organ damage over time. It’s not a quick fix. It takes 3 to 6 months to kick in. But when it does, the difference is real.
How Hydroxychloroquine Actually Works in the Body
Most drugs either kill something or block a receptor. Hydroxychloroquine works differently. It quietly interrupts the immune system’s false alarms.
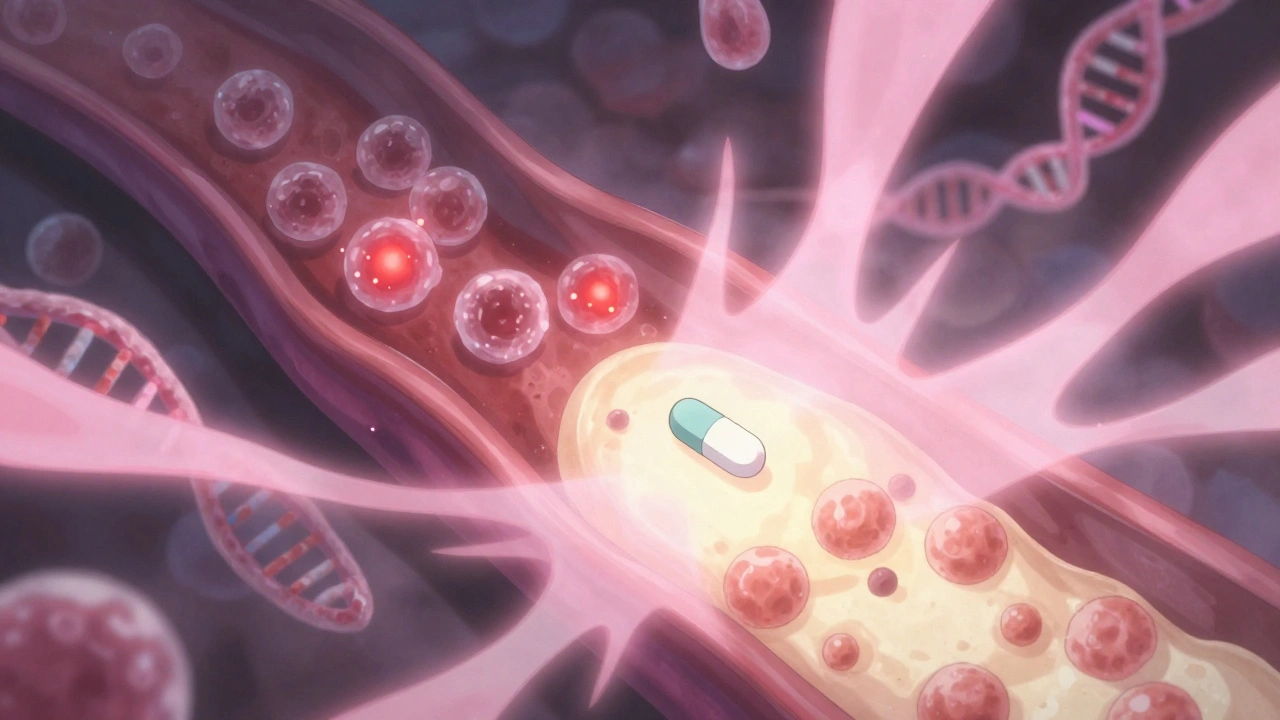
In lupus, your immune cells get confused. They think your own DNA and proteins are foreign invaders. This triggers a chain reaction: immune cells release inflammatory signals like interferons and TNF-alpha, which flood your joints and cause swelling. Hydroxychloroquine blocks this process at the source.
It enters immune cells and raises the pH inside their endosomes-tiny compartments where immune sensors like TLR7 and TLR9 normally activate. When these sensors can’t trigger properly, the immune system doesn’t sound the alarm. That means less interferon production (down by 35-40%), less TNF-alpha (down 25-30%), and fewer inflammatory cytokines like IL-1β and IL-6.
It also calms down another troublemaker: autophagy. In lupus, cells recycle their own components too aggressively, releasing more triggers for inflammation. Hydroxychloroquine slows this process by about 40% in animal models. And it reduces oxidative stress by blocking NADPH oxidase, cutting reactive oxygen species by 30-35%. These aren’t just lab effects-they translate to real-world relief.
How It Compares to Other Lupus Arthritis Treatments
There are other drugs for lupus arthritis. But none match hydroxychloroquine’s balance of safety, multi-system benefits, and cost.
- Methotrexate works better for severe joint swelling in some trials-but it’s harder on the liver. You need monthly blood tests. It can cause nausea, fatigue, and even lung problems in rare cases.
- Corticosteroids like prednisone give fast relief-sometimes in days. But long-term use? That’s a minefield. Bone loss, weight gain, diabetes, cataracts. One study found steroid users had a 40% higher risk of osteoporosis. Hydroxychloroquine? It actually helps preserve bone density.
- Biologics like belimumab or anifrolumab are powerful. They can reduce disease activity by 30-35%, more than hydroxychloroquine’s 20-25%. But they cost $45,000 a year. Hydroxychloroquine? Around $600-$1,200 annually, even with brand-name Plaquenil. Generics are even cheaper.
And here’s the kicker: hydroxychloroquine protects more than just your joints. It lowers your risk of blood clots by 30-35% in people with antiphospholipid syndrome. It improves cholesterol-raising good HDL by 5-10 mg/dL and lowering total cholesterol by 10-15 mg/dL. And it slashes infection risk. One study showed users had a 20-fold lower chance of serious infections than non-users.
Real Patient Stories: What It’s Like to Take Hydroxychloroquine
On forums like the Lupus Foundation of America’s community and Reddit’s r/lupus, people talk about hydroxychloroquine like it’s a lifeline.
One user, LupusWarrior87, wrote: “After 4 months on 300 mg, I went from needing 10 mg of prednisone every day to zero. My morning stiffness? Gone.”
Another, SLESurvivor, said: “It took five months to notice a difference. But two years in, I credit this drug for keeping me off high-dose steroids.”
Out of 3,542 patients surveyed on CreakyJoints, 76% said their joint swelling improved. Two-thirds reported fewer flares. But it’s not perfect. About a third reported side effects: vivid dreams (45%), nausea (30%), and anxiety about eye checks (25%).
That last one is real. People are scared of vision loss. And while it’s rare, it’s not imaginary.
The Eye Risk: What You Need to Know
The biggest concern with hydroxychloroquine is retinal toxicity. It’s uncommon, but it can be permanent.
Current guidelines say: get a baseline eye exam within the first year of starting the drug. Then, if you’re on a safe dose (≤5 mg per kg of body weight, max 400 mg/day) and have no other risk factors (like kidney disease or taking tamoxifen), you only need yearly exams after five years.
But here’s the catch: 7.5% of people on hydroxychloroquine for more than five years develop retinal changes. The key is staying under the dose limit. A 70 kg person should never take more than 350 mg daily. A 90 kg person? Max 400 mg.
New tools are helping. The FDA approved the AdaptDx Pro device in 2022-it detects early retinal changes before they show up on standard eye exams. It’s not in every clinic yet, but it’s reducing false negatives by 35%.
Most people never have issues. But skipping eye checks? That’s where the risk climbs.
Dosing, Timing, and What to Expect
Hydroxychloroquine doesn’t work overnight. It takes 3 to 6 months to reach full effect. That’s why so many people quit too soon. In one study, 25% stopped within the first year because they didn’t feel better fast enough.
Doctors usually start with 200 mg daily. If needed, they bump it to 400 mg. Dosing is based on real body weight-not ideal weight. A 62 kg person might take 300 mg daily. That’s 5 mg/kg.
It’s best taken with food to reduce stomach upset. Some people feel better taking it in the morning. Others take it at night to avoid dizziness. Vivid dreams are common but usually fade after a few weeks.
Don’t switch generic brands randomly. A 2022 JAMA study found some generics had 18% lower blood levels than others. Stick with the same manufacturer if you can.
Who Should Avoid It? And Who Benefits Most?
Hydroxychloroquine is safe for most people with lupus. Even pregnant women. Studies like PROMISSE show it’s safe for the baby and reduces the risk of preterm birth and flares during pregnancy. That’s why 78% of pregnant lupus patients take it.
It’s also used in 94% of pediatric lupus cases-better for growing bones than steroids.
But it’s not for everyone. If you have advanced retinal disease, severe liver disease, or a known allergy, skip it. If you’re on other drugs that affect the heart (like certain antibiotics or antidepressants), talk to your doctor. Hydroxychloroquine can rarely cause heart rhythm problems, especially at high cumulative doses.
And while it helps mild-to-moderate joint pain, it’s not strong enough for severe lupus nephritis. That needs mycophenolate or cyclophosphamide.
The Future of Hydroxychloroquine in Lupus
Even after 70 years, hydroxychloroquine keeps surprising researchers.
Recent studies suggest it may influence epigenetics-how your genes are turned on or off. It might also alter gut bacteria in ways that calm inflammation. A 2023 trial is testing it with a new biologic, anifrolumab, and early results show a 45% better response than hydroxychloroquine alone.
Doctors are now using blood tests to predict who will respond. One test looks at interferon gene signatures. If they normalize after 3 months on hydroxychloroquine, you’re likely to do well long-term.
It’s not a cure. But for most people with lupus arthritis, it’s the foundation. The drug that keeps flares at bay, protects your heart, saves your bones, and lets you live without constant steroids. It’s not flashy. It doesn’t make headlines. But for millions, it’s the quiet hero keeping them moving.


Hydroxychloroquine saved my wrists. Took six months, but now I can hold a coffee cup without wincing. No flares in two years. Simple as that.
It’s fascinating how a drug born from malaria treatment became the quiet architect of immune recalibration. Hydroxychloroquine doesn’t obliterate the fire-it rewires the alarm system. The body’s own DNA stops being labeled ‘enemy’ because the endosomal sensors are gently muffled. It’s not suppression. It’s diplomacy at the cellular level. And yet, we treat it like a placeholder drug. Maybe because it doesn’t come with a flashy IV drip or a six-figure price tag. But for those of us who’ve lived through steroid rollercoasters, it’s the only steady hand in the storm.
As someone from India where generic medications are lifelines, I’ve seen firsthand how hydroxychloroquine transforms lives without bankrupting families. In our rural clinics, patients on this drug report not just less joint pain but better sleep, less fatigue, and the rare luxury of planning a week ahead. The eye monitoring is non-negotiable, yes-but so is access. We need global equity here. This drug should be as available as aspirin in every lupus patient’s cabinet, not a privilege tied to insurance or geography.
Okay but the vivid dreams?? 😵💫 I swear I was fighting dragons in my sleep for three months. Also, why does everyone act like the eye thing is rare? My aunt went blind from it. Just saying.
Given the pleiotropic immunomodulatory effects mediated through TLR7/9 endosomal inhibition, coupled with downstream suppression of interferon-alpha and TNF-alpha cascades, it becomes evident that hydroxychloroquine functions as a master regulator of innate immune hyperactivity in SLE. The reduction in NADPH oxidase-derived ROS further corroborates its role in mitigating oxidative stress-induced inflammasome activation. However, the clinical translation of these molecular mechanisms remains underappreciated in primary care settings where symptom relief is prioritized over pathway analysis.
Man, I wish I’d known this 10 years ago. I was on prednisone like it was candy-until my hips started crumbling. Hydroxychloroquine didn’t fix me overnight, but it gave me back my life slowly, quietly. No drama. No IVs. Just a little pill that said, ‘Hey, you’re not broken, you’re just misfiring.’ And now? I hike. I garden. I don’t need a nap after brushing my teeth. Best decision I ever made.
lol so this is the ‘miracle drug’? I’ve been on it 3 years and still feel like a zombie. Also, my optometrist charges $200 for every eye check. Who even has time for this?
It’s interesting how the narrative around hydroxychloroquine has shifted so dramatically over the past decade-from being dismissed as an old-school antimalarial to now being recognized as a foundational immunomodulator in systemic autoimmune disease. The pharmacokinetics are relatively straightforward, but the downstream epigenetic and microbiome interactions are still poorly understood. What’s more concerning is the lack of longitudinal data beyond ten years of use, particularly regarding cumulative retinal toxicity thresholds in patients with comorbid metabolic syndrome. Many studies focus on efficacy in mild-to-moderate disease, yet we have little insight into its role in refractory cases where biologics are already in play.
While the anecdotal testimonials are emotionally compelling, one must interrogate the methodological rigor of the CreakyJoints survey-self-reported outcomes, selection bias, absence of control groups. Furthermore, the assertion that hydroxychloroquine reduces infection risk by 20-fold is statistically dubious without multivariate adjustment for confounding variables such as concomitant immunosuppressant use. The medical literature does not support such an extreme claim.
How quaint. A 1940s antimalarial, repurposed like a relic from a bygone era, now hailed as the ‘quiet hero’ of lupus care. How utterly… pedestrian. One wonders if the medical establishment has simply run out of imagination-or perhaps, the pharmaceutical industry has. Truly, the pinnacle of innovation: a $600 pill that works because it doesn’t try too hard. How very… American.
There’s something almost poetic about HCQ’s understated efficacy-like a monk whispering truths while the world screams for fireworks. The retinal toxicity risk? A necessary cost of epistemic humility. We want miracles, but we’re too lazy to show up for yearly eye exams. The real tragedy isn’t the drug-it’s our collective refusal to engage with slow, steady healing. Also, the AdaptDx Pro? Brilliant. Why isn’t it in every optometrist’s office yet? 🤔
Recent studies on interferon gene signatures as predictive biomarkers for HCQ response are groundbreaking. If we can stratify patients early-those with high IFN signatures likely to respond-this could shift HCQ from empirical to precision therapy. Imagine a blood test at diagnosis that tells you, ‘This drug will work for you.’ No more six-month wait-and-see. That’s the future.
And yet… we still don’t know if it prevents cancer. Or dementia. Or heart disease. It’s just… arthritis. That’s it. Why is everyone acting like it’s the second coming?!