Opioid Patches: How They Work, Risks, and Alternatives for Pain Management
When you hear opioid patches, transdermal delivery systems that release controlled doses of strong painkillers through the skin. Also known as fentanyl patches, they’re designed for chronic, around-the-clock pain—not sudden flare-ups. Unlike pills that hit hard and fade fast, these patches slowly leak medication into your bloodstream over days. That’s why doctors use them for cancer pain, severe arthritis, or long-term nerve damage. But they’re not harmless. A single patch can contain enough opioid to kill someone who’s never taken one before.
They work by sticking to your skin—usually on the chest, back, or upper arm—and letting the drug seep in over 72 hours. That steady release helps avoid the highs and crashes you get with oral opioids. But if the patch gets too warm—say, from a heating pad, hot bath, or fever—the drug flows faster. That’s how overdoses happen. And because they’re invisible and long-lasting, people often forget they’re even wearing one. That’s dangerous when you’re also taking sleep aids, anxiety meds, or alcohol. The fentanyl patch, the most common type of opioid patch. Also known as Duragesic, it’s powerful enough to require strict monitoring. Even if you’ve used it for months, your body doesn’t get used to the risk. Tolerance builds for pain relief, but not for respiratory depression.
That’s why many people switch to safer options. Topical NSAIDs like diclofenac gel can handle arthritis pain without touching your brain. Capsaicin cream works by burning out pain nerves over time. And for nerve pain, gabapentin or pregabalin often do the job without addiction risk. Some patients find relief with physical therapy, acupuncture, or even low-dose antidepressants that calm nerve signals. These don’t fix everything, but they avoid the opioid trap. The real question isn’t just whether patches work—it’s whether they’re the *least bad* choice for you.
Below, you’ll find real comparisons of pain treatments that actually matter. From how to safely dispose of used patches to what happens when you stop them cold, these guides cut through the noise. You’ll see what works for others, what doesn’t, and how to talk to your doctor about options that keep you in control—not the other way around.
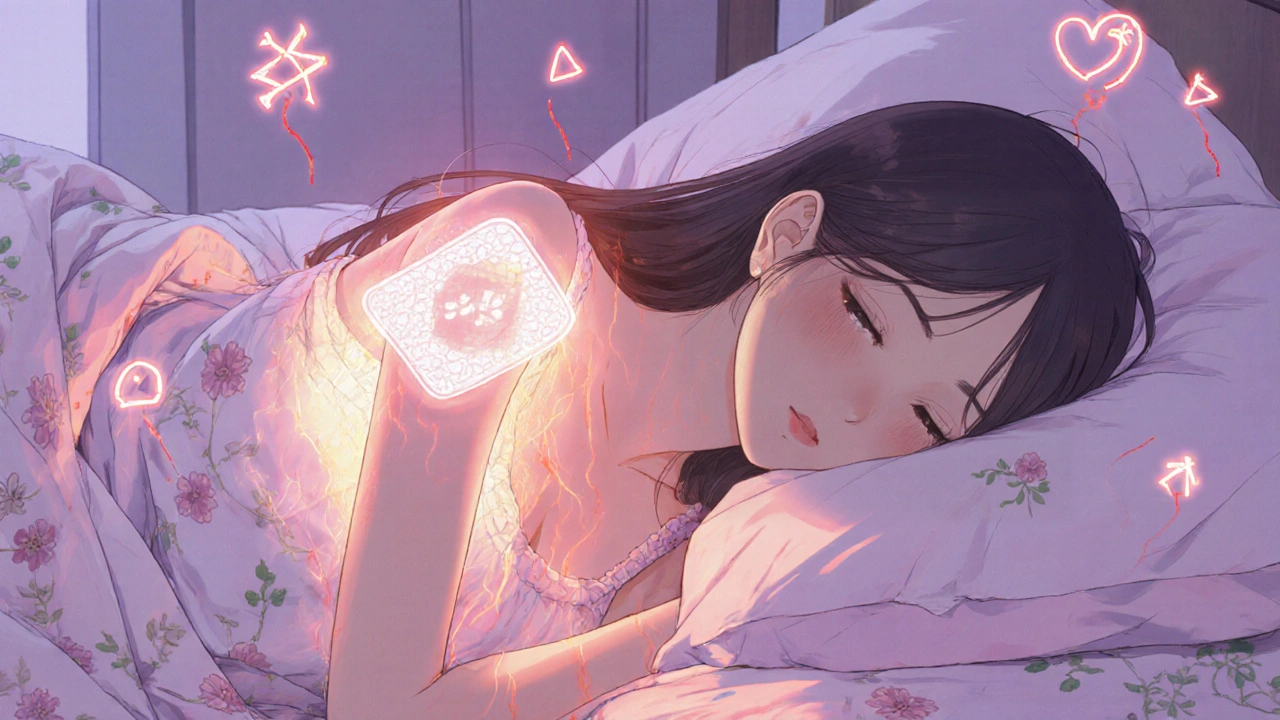
Heat and Fentanyl Patches: How Heat Increases Overdose Risk
Fentanyl patches can be life-saving for chronic pain-but heat can turn them deadly. Learn how temperature changes increase overdose risk and what you must avoid to stay safe.
- Drug Information (70)
- Health and Wellness (59)
- Pharmacy Information (25)
- Medical Conditions (24)
- Supplements (4)
- Diabetes (4)
- Travel Health (3)
- Mental Health (3)
- Heart Health (2)
- Parenting (2)
-
Global Generic Drug Policies: How Countries Balance Affordability and Quality
5 Feb 2026 -
Sarcopenia: How Strength Training Slows Age-Related Muscle Loss
10 Dec 2025 -
Dental Prophylaxis for Children: Establishing Good Oral Hygiene Habits Early
27 Jun 2023 -
How Velpatasvir is Revolutionizing the Treatment of Hepatitis C
29 Apr 2023 -
Clavulanic Acid: Addressing the Challenges of Antibiotic Resistance
5 May 2023

1.11.25
Alistair Mukondiwa
7