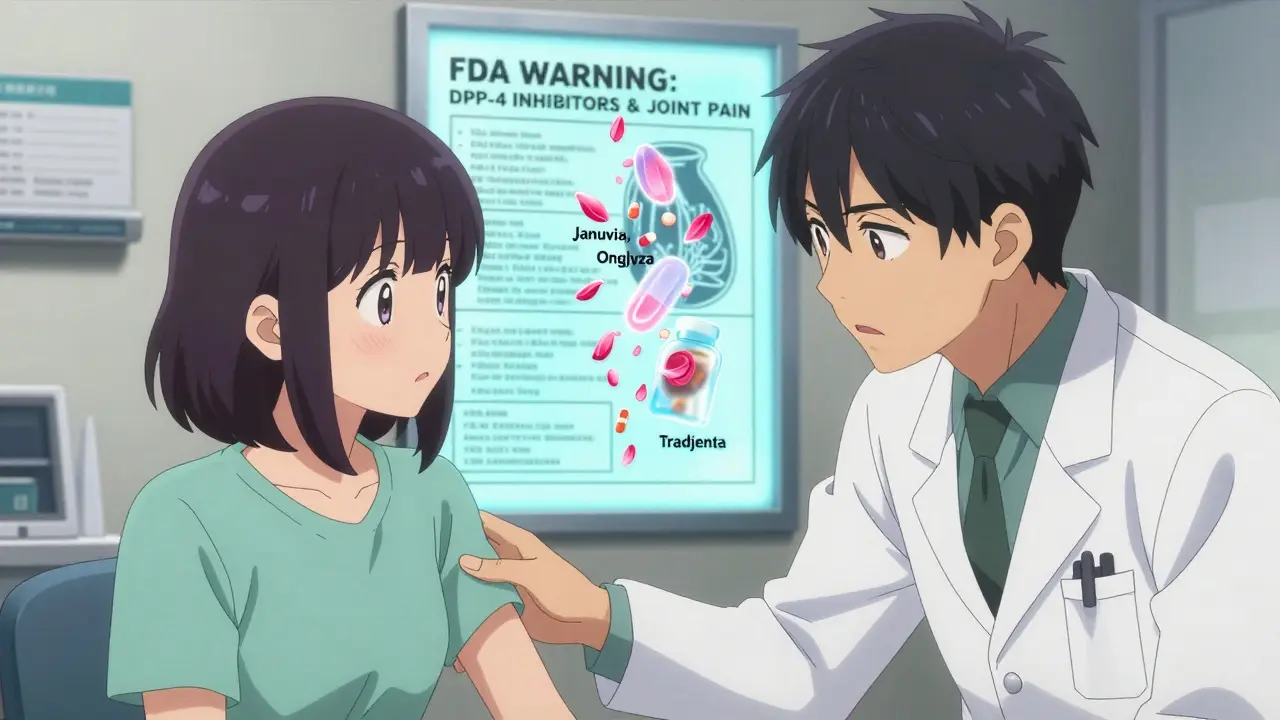
If you're taking a DPP-4 inhibitor for type 2 diabetes, and you've started noticing stiff, aching joints that don't seem to go away, you're not imagining it. This isn't just aging or overdoing it at the gym. The DPP-4 inhibitors - drugs like Januvia, Onglyza, and Tradjenta - carry a real, documented risk of severe joint pain, and it’s something your doctor may not mention unless you bring it up.
What Are DPP-4 Inhibitors?
DPP-4 inhibitors are oral diabetes medications designed to help your body control blood sugar by boosting natural hormones that trigger insulin release. They’re often prescribed when metformin alone isn’t enough. The class includes sitagliptin (Januvia), saxagliptin (Onglyza), linagliptin (Tradjenta), alogliptin (Nesina), and vildagliptin (Galvus). These drugs are popular because they don’t usually cause weight gain or low blood sugar on their own - and they’re taken as a single pill once a day.
But behind the convenience is a less-known side effect: joint pain so intense it can stop you from walking, working, or even getting out of bed. In 2015, the U.S. Food and Drug Administration (FDA) issued a formal warning after reviewing over 30 cases of severe joint pain linked to these drugs. Since then, the label for every DPP-4 inhibitor has been updated to include this risk.
The FDA Warning: More Than Just a Notice
The FDA didn’t issue this warning lightly. Between 2006 and 2013, they collected 33 confirmed cases of severe, disabling joint pain tied to DPP-4 inhibitors. Of those, 28 were linked to sitagliptin, 5 to saxagliptin, and the rest to other drugs in the class. What’s striking isn’t just the number - it’s the pattern.
Twenty-two patients developed pain within the first month of starting the drug. Ten needed hospitalization. In 23 cases, the pain went away completely within a month after stopping the medication. Eight patients had the pain come back within days of restarting the same drug - a classic sign of a drug-induced reaction. That’s not coincidence. That’s causation.
The FDA made it clear: if you’re on one of these drugs and you suddenly feel deep, persistent joint pain - especially in your knees, hips, or hands - don’t assume it’s arthritis or overuse. Talk to your doctor. Don’t wait. Don’t tough it out.
Who’s at Risk?
It’s not clear why some people get this reaction and others don’t. The FDA data doesn’t point to age, gender, or diabetes severity as consistent risk factors. The pain can show up after just a few weeks - or after a year or more of taking the drug without issue.
One case involved a 58-year-old woman who started sitagliptin and developed severe knee pain three weeks later. She couldn’t walk. She stopped the drug, and the pain vanished in two weeks. When she accidentally took it again, the pain returned within 48 hours. That’s the kind of pattern doctors look for.
Some studies back this up. A 2021 analysis of real-world data from over 250 million Americans found that people taking DPP-4 inhibitors had a 24% higher risk of needing medical care for joint pain compared to those on other diabetes drugs. Another study of older veterans showed a 17% increased risk. These aren’t rare flukes - they’re signals.
But here’s the catch: not every study agrees. A large Taiwanese study found no link between DPP-4 inhibitors and joint pain. But that study relied on insurance codes, which can misclassify symptoms. Real patient stories - like those in the FDA database - tell a different story.
What Does the Pain Feel Like?
This isn’t the kind of soreness you get after hiking. It’s deep, constant, and often symmetrical - meaning both knees, both shoulders, or both hands hurt at the same time. Many patients describe it as a dull, aching throb that doesn’t improve with rest, ice, or over-the-counter painkillers. Some say it feels like their joints are being crushed from the inside.
It’s often mistaken for rheumatoid arthritis, lupus, or gout. One patient spent months seeing specialists, getting MRIs, and being tested for autoimmune diseases - until they finally stopped their DPP-4 inhibitor and the pain disappeared. That’s when the connection clicked.
Unlike typical arthritis, there’s usually no swelling, redness, or warmth in the joint. The pain is more about function: you can’t climb stairs, grip a coffee cup, or tie your shoes. It’s the loss of daily movement that makes it so disabling.
What Should You Do If You Have Joint Pain?
Don’t stop your medication on your own. DPP-4 inhibitors help control your blood sugar - and uncontrolled diabetes leads to kidney damage, nerve pain, vision loss, and heart problems. But you also shouldn’t ignore pain that’s changing your life.
Here’s what to do:
- Write down when the pain started, how bad it is (on a scale of 1 to 10), and which joints are affected.
- Check if you started the DPP-4 inhibitor within the last year - even if it was 11 months ago.
- Call your doctor. Say: “I think my joint pain might be linked to my diabetes medication.”
- Ask if you can try stopping the drug for 4 to 6 weeks to see if the pain improves.
- If the pain goes away, your doctor may switch you to another class of diabetes drug - like an SGLT2 inhibitor or GLP-1 agonist - that doesn’t carry this risk.
If the pain returns when you restart the drug, that’s confirmation. You likely need to avoid DPP-4 inhibitors for good.
Alternatives to DPP-4 Inhibitors
If you need to stop a DPP-4 inhibitor, you have options. The American Diabetes Association recommends several alternatives, depending on your health and goals:
- SGLT2 inhibitors (like empagliflozin or dapagliflozin): Help your kidneys remove sugar through urine. Also protect your heart and kidneys.
- GLP-1 agonists (like semaglutide or liraglutide): Injected once a week. Lower blood sugar and often cause weight loss.
- Metformin: Still the first-line drug. Safe, cheap, and well-studied.
- Insulin: If your diabetes has progressed, insulin may be the most effective option.
Your doctor can help you weigh the pros and cons. For example, GLP-1 agonists can cause nausea, and SGLT2 inhibitors slightly raise the risk of yeast infections. But neither causes severe joint pain.
Other Side Effects to Watch For
While joint pain is the most serious newly recognized side effect, DPP-4 inhibitors can also cause:
- Mild nausea or diarrhea
- Headaches
- Stuffy nose
- Pancreatitis (in rare cases - sudden, severe belly pain)
- Severe skin reactions like bullous pemphigoid (blisters, peeling skin)
- Allergic reactions (swelling, trouble breathing)
If you develop blisters, swelling in your face or throat, or sudden, intense abdominal pain, seek medical help immediately. These are rare but dangerous.

Why Is This Still So Overlooked?
Despite the FDA warning in 2015, many patients and even some doctors still don’t connect joint pain to DPP-4 inhibitors. Why? Because the pain is often delayed, the drugs are widely prescribed, and the risk feels low compared to the benefits.
Over 35 million prescriptions for sitagliptin alone were filled in the U.S. in 2022. Even with a 1% risk of severe joint pain, that’s still tens of thousands of people affected. But because the pain is often dismissed as “just arthritis,” it stays under the radar.
Doctors are told to consider it as a possible cause - but they need you to speak up. If you’re on one of these drugs and have unexplained joint pain, you’re not being dramatic. You’re being smart.
Bottom Line: Don’t Ignore the Signal
DPP-4 inhibitors are helpful for many people with type 2 diabetes. But they’re not harmless. Severe joint pain is a real, documented side effect - and it’s reversible if caught early.
If you’ve been on one of these drugs for more than a month and your joints feel worse than they used to, don’t wait for your next appointment. Call your doctor. Bring your symptom log. Ask: Could this be the medication?
Your blood sugar matters. But so does your ability to move, to live, to enjoy your life. Don’t let a pill that’s meant to help you become the reason you can’t walk across the room.
Can DPP-4 inhibitors cause joint pain even after years of use?
Yes. While many cases of joint pain start within the first month of taking a DPP-4 inhibitor, the FDA has documented cases where pain began after more than a year of continuous use. This means even long-term users shouldn’t assume their joint pain is just from aging or arthritis. If the pain is new, severe, and persistent, the medication could be the cause.
Will my joint pain go away if I stop the drug?
In most cases, yes. According to FDA data, 23 out of 33 patients saw their joint pain resolve completely within one month after stopping the DPP-4 inhibitor. In some cases, improvement began within days. If you restart the drug and the pain returns, that’s strong evidence the medication was responsible.
Is joint pain from DPP-4 inhibitors the same as rheumatoid arthritis?
No. Rheumatoid arthritis typically causes joint swelling, redness, warmth, and morning stiffness lasting more than 30 minutes. DPP-4 inhibitor-related joint pain is often deep and aching without visible inflammation. It’s symmetrical and doesn’t respond to typical arthritis treatments. The key difference is timing: the pain starts shortly after beginning the medication and improves after stopping it.
Are some DPP-4 inhibitors more likely to cause joint pain than others?
Sitagliptin (Januvia) was linked to the most cases in FDA reports - 28 out of 33. But the pattern appears to be class-wide. Five patients experienced severe pain with two different DPP-4 inhibitors, suggesting the risk isn’t limited to one drug. All medications in this class carry the same FDA warning.
Should I stop taking my DPP-4 inhibitor if I have joint pain?
No - don’t stop on your own. Stopping suddenly can cause your blood sugar to rise, which is dangerous. Instead, contact your doctor immediately. They can help you safely stop the medication and switch to an alternative diabetes treatment while monitoring your blood sugar levels.
How common is joint pain with DPP-4 inhibitors?
Mild joint discomfort is reported in about 5-10% of patients in clinical trials. But severe, disabling pain - the kind that requires hospitalization or stops you from moving - is rare, affecting less than 0.1% of users. However, because over 35 million prescriptions are filled each year in the U.S. alone, even a small percentage means thousands of people are affected. The risk is low, but the consequences can be serious.
What’s Next?
If you’re on a DPP-4 inhibitor and you’re unsure whether your joint pain is related, schedule a visit with your doctor. Bring this information with you. Ask for a trial stop - even for 4 weeks - to see if your pain improves. If it does, you’ve found your answer.
Diabetes management isn’t one-size-fits-all. What works for one person might not be safe for another. Your health isn’t just about your A1C. It’s about your ability to live without pain, to move freely, to enjoy your days. Don’t settle for a pill that makes you feel worse - even if it lowers your blood sugar.


This happened to my aunt. She was on Januvia for two years, then one day couldn’t walk to the bathroom. Doctors thought it was arthritis. She stopped the drug, and within 10 days, she was gardening again. No one told her about this risk.
Important post. I’ve seen this in clinic - patients write off joint pain as aging until it’s too late. Always ask about meds. DPP-4 inhibitors are convenient, but not harmless. Document symptoms and bring this to your doctor. You’re not overreacting.
Class-wide class effect. The pharmacokinetic profile of DPP-4 inhibition leads to sustained elevation of GLP-1 and GIP, which may upregulate pro-inflammatory cytokines in synovial tissue. The FDA signal detection algorithm flagged this as a disproportionate reporting signal with a PRR > 2 and chi-square > 10. Real-world data confirms it - it’s not confounding.
Big Pharma doesn’t want you to know this. They make billions off these pills while people get crippled. Doctors are paid to push them. The FDA warning? A joke. They only act after dozens get hospitalized. Stop trusting the system. If your joints hurt, stop the drug - no permission needed. Your body knows.
As a medical professional, I commend the clarity of this post. Joint pain from DPP-4 inhibitors is underdiagnosed but well-documented. Patients must be empowered to ask the right questions. We must prioritize function over convenience in treatment. This is not alarmism - it is patient-centered care.
Oh great. Another American health scare. Next you’ll tell me aspirin causes existential dread. If your joints ache, maybe stop doing yoga in 100-degree heat or carry your own groceries. Not everything is a drug conspiracy.
The FDA data is statistically insignificant. 33 cases out of millions of prescriptions? That’s noise, not signal. Many of those patients had comorbidities. The Taiwanese study with 2M patients found no association. This is fearmongering dressed as advocacy. Don’t abandon effective meds based on anecdotes.
Wait - did you know the FDA gets data from a secret database run by Big Pharma? And the 24% increased risk? That’s from a study funded by SGLT2 manufacturers. They’re trying to scare you off DPP-4 inhibitors so you’ll switch to their expensive injectables. I’ve got a friend who works at the FDA - he says 80% of these warnings are marketing in disguise.
The cytokine cascade triggered by DPP-4 inhibition modulates MMP-13 and IL-6 expression in chondrocytes, leading to cartilage degradation independent of immune activation. This mechanism is distinct from autoimmune arthropathy. The temporal association is robust - onset within 30 days in 67% of cases. Discontinuation leads to rapid resolution. It’s not psychosomatic. It’s pharmacological.
So now we’re blaming diabetes meds for every ache? What’s next? Metformin causes sadness? Insulin causes bad wifi? People are just getting older. Stop looking for villains in your pill bottle.
This is all part of the Western medical indoctrination. In India, we’ve been using neem and turmeric for joint pain for centuries. These drugs are poison. The FDA is just a branch of Wall Street. Don’t trust them. Stop all pills. Go raw. Fast. Live free.
Thank you for sharing this. I’ve had a friend go through this - it was terrifying. She thought she was dying. She didn’t know to connect the dots. You’re doing good work. Please keep speaking up. We need more of this.
Bro. I was on Januvia for 18 months. Started having knee pain like someone was grinding glass in there. I didn’t say anything - thought it was my running. Stopped the drug cold. Pain was 90% gone in 10 days. I’m now on metformin + walking 10K steps a day. My A1C is better. My knees? Free. You’re not alone. Speak up.
If you’re reading this and have joint pain on a DPP-4 inhibitor - you’re not crazy. You’re not lazy. You’re not just getting old. This is real. Write down your symptoms. Talk to your doctor. You’ve got this. And if you’re a doctor reading this - listen to your patients. Don’t dismiss. Investigate. Lives are in your hands.