Bromhexine – Complete Guide
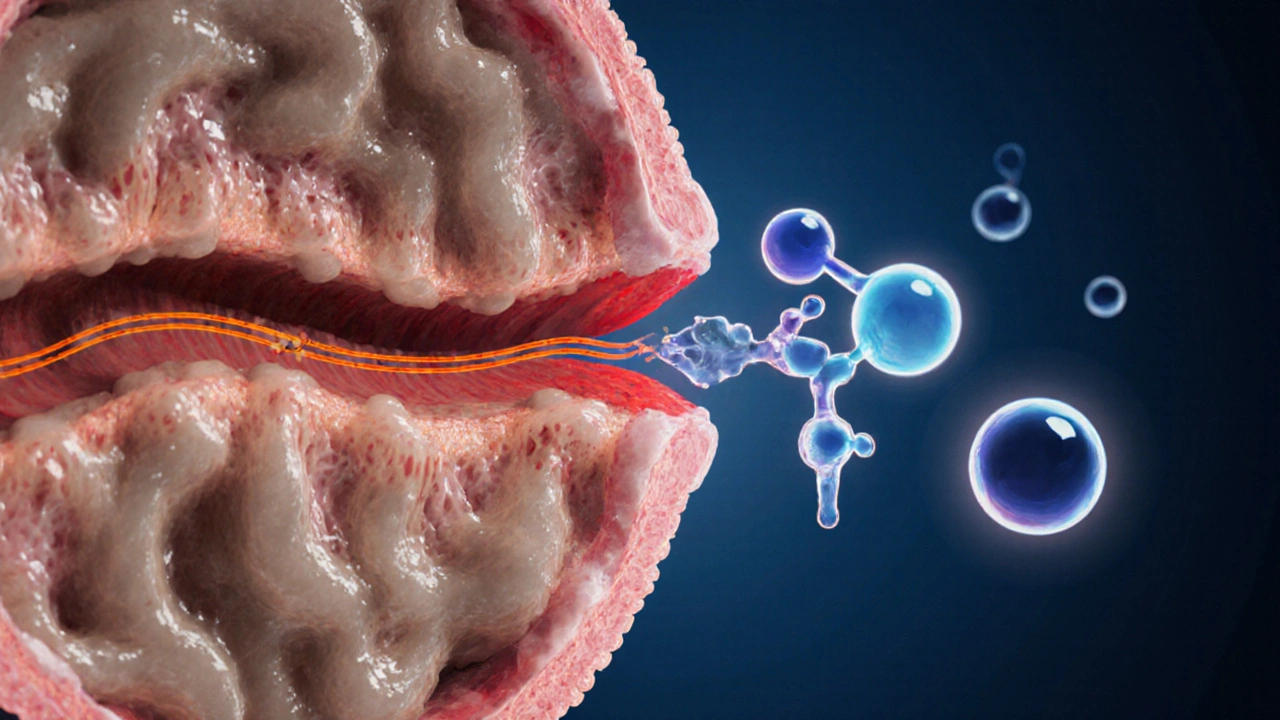
When working with bromhexine, a mucolytic agent that thins airway mucus, making it easier to clear from the lungs. Also known as Bisolvon, it is frequently prescribed for bronchitis, pneumonia and other respiratory infections.
In the same breath, mucolytic, any drug that reduces the viscosity of mucus to improve airway patency is the broader class that houses bromhexine. Another closely related class is the expectorant, a medication that stimulates cough reflexes to expel loosened secretions. While both classes aim to clear mucus, mucolytics act on the molecular structure of the mucus, and expectorants trigger the mechanical act of coughing. Understanding how these categories interact helps you pick the right combination for a stubborn cough.
Key considerations for using bromhexine
First off, bromhexine works by stimulating the serous cells in the respiratory tract to produce thinner secretions and by breaking disulfide bonds in mucus proteins. This dual action means you get clearer airways faster than with a plain expectorant alone. Typical adult dosing is 8 mg three times daily, but pediatric doses are weight‑based – usually 2 mg per kilogram per day divided into three doses. It’s best taken after meals to minimize stomach upset, a common side effect.
Safety-wise, bromhexine has a low incidence of serious adverse events. The most reported issues are mild nausea, abdominal discomfort, or rare allergic reactions like rash and itching. Because it’s metabolized in the liver, patients with severe hepatic impairment should use it cautiously or avoid it. Drug‑drug interactions are limited, but combining it with strong CYP3A4 inhibitors (e.g., ketoconazole) may raise plasma levels slightly, so monitoring is advised.
When choosing a therapy, consider the infection type. For acute bronchitis caused by viral pathogens, using bromhexine together with an expectorant such as guaifenesin can speed up mucus clearance and reduce cough duration. In chronic obstructive pulmonary disease (COPD), regular mucolytic therapy including bromhexine helps maintain airway openness and may lower exacerbation rates. If you’re already on an inhaled bronchodilator, adding bromhexine does not interfere with its action, making it a safe add‑on.
One practical tip many users overlook: hydration amplifies bromhexine’s effect. Drinking plenty of fluids provides the necessary water to keep mucus thin, turning the drug’s chemical work into a physical result you can feel when you cough. Conversely, dehydration can blunt its benefits and keep secretions stubbornly thick.
For patients with asthma, bromhexine is generally well‑tolerated, but it should never replace a rescue inhaler. It can, however, serve as a maintenance aid during flare‑ups when mucus plugs are the main problem. Always discuss with a healthcare professional before starting, especially if you’re pregnant, nursing, or on anticoagulants, as the data on bleeding risk is limited.
Finally, the market offers several bromhexine formulations: syrup, tablets, and lozenges. Syrup is popular for children because it’s easy to dose, while tablets suit adults looking for convenience. Lozenges provide a slow release that can be handy for night‑time coughing. Choose the form that matches your lifestyle and stick to the recommended regimen for consistent results.
Below you’ll find a curated collection of articles that dive deeper into specific scenarios – from using bromhexine with other cough medicines, to dosing guidelines for seniors, to safety checklists for travel‑related respiratory infections. Each piece offers actionable advice you can apply right away, so keep reading to get the most out of your bromhexine therapy.
Carbocisteine vs Other Mucolytics: Detailed Comparison and Alternatives
A thorough comparison of Carbocisteine with Ambroxol, N‑acetylcysteine, bromhexine and guaifenesin, covering mechanisms, dosage, side effects, cost and when each is best to use.
- Drug Information (69)
- Health and Wellness (59)
- Medical Conditions (22)
- Pharmacy Information (22)
- Supplements (4)
- Diabetes (4)
- Travel Health (3)
- Mental Health (3)
- Heart Health (2)
- Parenting (2)
-
Azelaic Acid Benefits for Mature Skin: Anti‑Aging, Brightening & Gentle Care
19 Oct 2025 -
Nimotop vs. Alternative Calcium Channel Blockers: A Practical Comparison
28 Sep 2025 -
Pharmacy Reimbursement Models: How Laws Shape Generic Drug Payments
16 Nov 2025 -
Antidepressants and Birth Control: What You Need to Know About Medication Interactions
24 Nov 2025 -
Out-of-Pocket Costs: What Patients Really Pay for Generic vs Brand-Name Drugs
27 Jan 2026

14.10.25
Alistair Mukondiwa
19