When it comes to loosening thick airway mucus, Carbocisteine is a widely prescribed synthetic mucolytic that reduces mucus viscosity by breaking disulfide bonds in mucoproteins. If you’ve ever wondered whether another drug might work faster, cause fewer side effects, or be easier to find in a pharmacy, you’re in the right place. This guide lines up the most common alternatives - Ambroxol, N‑acetylcysteine, bromhexine, and guaifenesin - and puts Carbocisteine side‑by‑side with each on the factors that matter to patients and clinicians alike.
How Carbocisteine Works
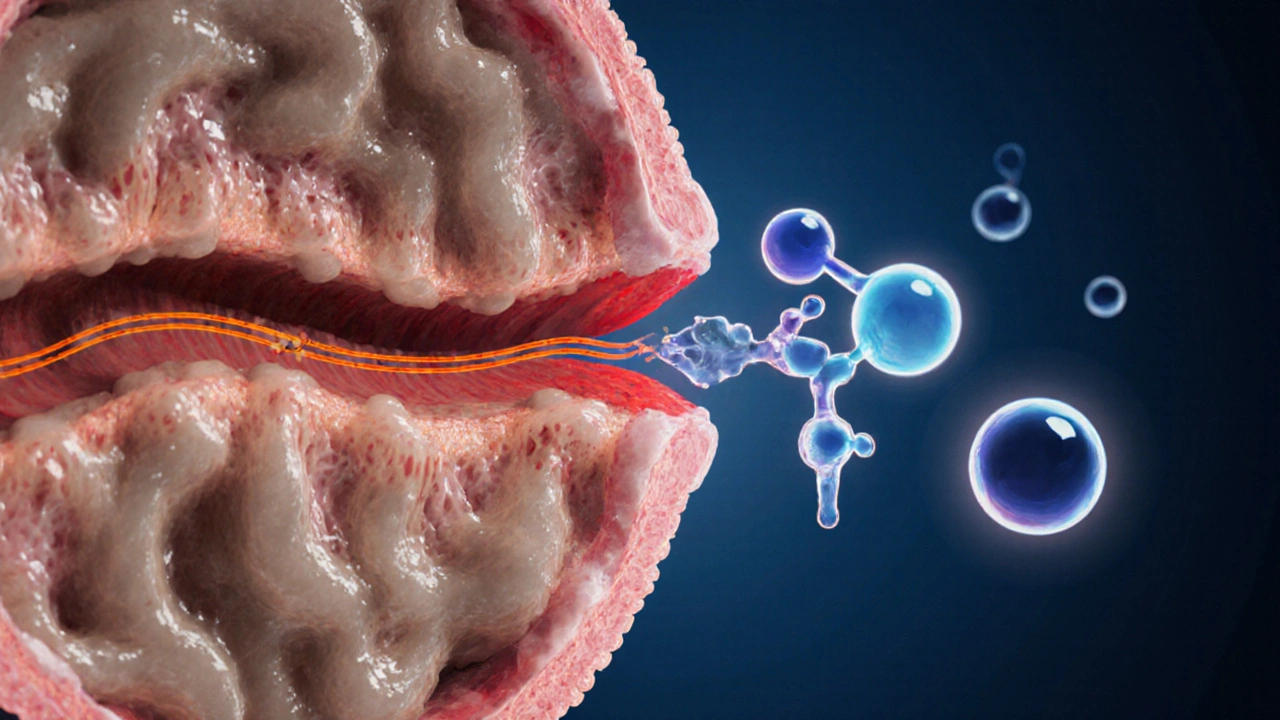
Carbocisteine belongs to the Mucolytic class. Its core action is to cleave the sulphide bridges that give mucus its sticky, gel‑like texture. By doing so, the drug turns thick secretions into a more fluid form that cilia can move up the respiratory tract. Typical adult dosing for chronic bronchitis is 500mg three times daily, taken after meals to reduce gastrointestinal irritation.
What Are the Main Alternatives?
Below is a quick snapshot of the four most common alternatives you’ll encounter in Australia and many other markets.
- Ambroxol - a derivative of bromhexine that stimulates serous gland secretion and increases ciliary beat frequency.
- N‑acetylcysteine (often abbreviated NAC) - provides a direct source of cysteine, replenishing glutathione and breaking disulphide bonds.
- Bromhexine - the parent compound of ambroxol, works by depolymerising mucopolysaccharide fibers.
- Guaifenesin - an expectorant that hydrates airway secretions but does not chemically alter mucin structure.
Key Comparison Factors
When you’re comparing mucolytics, focus on these six criteria. They cover efficacy, speed of onset, safety, dosing convenience, drug‑interaction risk, and availability in Australian pharmacies.
- Efficacy in reducing mucus viscosity
- Onset of symptom relief
- Side‑effect profile
- Typical dosage schedule
- Known drug interactions
- Prescription vs. over‑the‑counter status
Side‑by‑Side Comparison Table
| Attribute | Carbocisteine | Ambroxol | N‑acetylcysteine | Bromhexine | Guaifenesin |
|---|---|---|---|---|---|
| Mechanism | Breaks disulfide bonds in mucoproteins | Increases serous secretion & ciliary beat | Supplies cysteine → glutathione boost | Depolymerises mucopolysaccharide fibers | Hydrates mucus, promotes expectoration |
| Typical Dose (adult) | 500mg×3daily | 30mg×3daily | 600mg×2daily (oral) or 3‑5mL nebulised | 8mg×3daily | 200-400mg×4daily |
| Onset of Relief | 4-6hours | 30-60minutes | 45-90minutes (oral) | 1-2hours | 1‑2hours |
| Common Side Effects | GI upset, rash | Metallic taste, mild nausea | Bad taste, occasional bronchospasm | Headache, dizziness | GI discomfort, dizziness |
| Prescription Status (AU) | Prescription | Prescription | Prescription (nebulised) / OTC (oral) | Prescription | OTC |
| Notable Interactions | Antacids may reduce absorption | Bronchodilators - additive effect | Nitroglycerin - risk of hypotension | Warfarin - potential increase | None clinically significant |

When Carbocisteine Is the Better Choice
If you have chronic bronchitis with persistent, thick sputum, Carbocisteine’s strong mucolytic action can be more effective than an expectorant like guaifenesin. Its three‑times‑daily schedule keeps mucus consistently thin, which is helpful for patients who need steady control rather than a rapid, short‑term boost. Moreover, because it does not rely on stimulating airway secretions, it’s less likely to cause cough reflex irritation in sensitive individuals.
When Alternatives Shine
Ambroxol’s rapid onset (often within an hour) makes it a go‑to for acute exacerbations of COPD where you need quick relief. N‑acetylcysteine is unique because it also replenishes lung antioxidant defenses, a bonus for smokers or patients with oxidative stress‑related lung injury. Bromhexine offers a middle ground - decent mucolysis with a slightly lower pill burden than Carbocisteine. Guaifenesin, being over‑the‑counter, is convenient for mild, occasional chest congestion without the need for a prescription.
Safety and Contra‑indications
All mucolytics share a baseline risk of gastrointestinal upset, but the severity varies. Carbocisteine can provoke rash in patients with a history of drug‑related skin reactions. Ambroxol is generally well tolerated, yet the metallic taste can be off‑putting for some. N‑acetylcysteine’s sulphuric odor and occasional bronchospasm mean it should be introduced cautiously in asthma patients.
A key safety tip: always review current medications for potential interactions. For example, if you’re on warfarin, bromhexine could increase bleeding risk, so monitoring INR levels is advisable.
Practical Tips for Using Mucolytics
- Take Carbocisteine with food to minimise stomach irritation.
- Ambroxol works best when the dose is spaced evenly across the day - avoid taking it right before bedtime if the metallic taste wakes you.
- For N‑acetylcysteine nebulisation, use a calibrated compressor to ensure the mist is fine enough to reach peripheral airways.
- Bromhexine should be swallowed whole; crushing can alter the release profile.
- Guaifenesin benefits from plenty of water intake - the fluid helps thin mucus further.

Cost and Accessibility in Australia
Prescription mucolytics like Carbocisteine, Ambroxol, and bromhexine are typically subsidised under the PBS (Pharmaceutical Benefits Scheme) for eligible patients, bringing the out‑of‑pocket cost down to around $6-$9 per pack. N‑acetylcysteine oral forms are also PBS‑listed, while the nebulised solution may incur higher fees. Guaifenesin, being OTC, is priced between $8 and $15 for a month’s supply, depending on brand.
Choosing the Right Agent - A Quick Decision Flow
Use the following simple flowchart to narrow down your choice:
- Is rapid symptom relief (<1hour) essential? → Ambroxol.
- Do you need antioxidant support for smoking‑related damage? → N‑acetylcysteine.
- Is a prescription acceptable and you need consistent mucus thinning? → Carbocisteine.
- Is cost a primary concern and you can manage with milder effect? → Guaifenesin.
- Do you have a history of drug‑induced rash? → Avoid Carbocisteine, consider Ambroxol or bromhexine.
Future Directions in Mucolytic Therapy
Research in 2024-2025 is exploring combination products-pairing a classic mucolytic like Carbocisteine with a short‑acting bronchodilator in a single inhaler. Early trials suggest improved patient adherence and a modest increase in lung function metrics (FEV₁ rise of 5‑7%). Keep an eye on upcoming PBS listings for these combos, as they could reshape standard care for chronic bronchitis and COPD.
Frequently Asked Questions
Can I switch from Carbocisteine to an over‑the‑counter product?
Yes, but only after discussing with your doctor. Over‑the‑counter options like guaifenesin are milder and may not provide the same level of mucus thinning needed for chronic conditions. A gradual taper is usually recommended to avoid rebound mucus buildup.
Is Carbocisteine safe for pregnant women?
Limited human data exist, but animal studies have not shown teratogenic effects. Australian guidelines advise using the lowest effective dose only if the benefits outweigh potential risks, and always under clinician supervision.
How long does it take to see improvement with Carbocisteine?
Most patients report noticeable thinning of sputum within 4-6hours after the first dose, with maximal effect after 2‑3days of regular dosing.
Are there any foods or drinks I should avoid while taking Carbocisteine?
Alcohol can increase stomach irritation, and antacids may reduce absorption. It’s best to take the medication with a light meal and avoid high‑acid beverages right before dosing.
Can children use Carbocisteine?
Carbocisteine is approved for children over 6years in Australia, with the dose adjusted by weight (typically 10mg/kg three times daily). Always confirm the exact dose with a pediatrician.

Reading through the mucolytic comparison feels like a small philosophical journey into how we manipulate the very chemistry of our breath 😊. Carbocisteine, with its disulfide‑cleaving action, exemplifies a rational approach to thinning mucus, and that logical precision is commendable. Yet the rapid onset of ambroxol or the antioxidant boost from N‑acetylcysteine reminds us that speed and resilience matter just as much. Optimistically, clinicians can tailor therapy to each patient’s needs, harnessing the strengths of every agent. Let’s champion informed choice and not settle for a one‑size‑fits‑all solution! 🚀
One might wonder whether the pharmaceutical giants are quietly steering us toward a specific mucolytic, subtly embedding hidden agendas within the prescription pads. The data on side‑effects feels curated, as if the real risks are being filtered out of public view. It is unsettling to think that even the “OTC” status of guaifenesin could be a façade, designed to funnel patients into a larger network of controlled substances. Yet, I also sense a personal responsibility to dissect these claims, to resist the invisible hand that pulls the strings. In the end, the truth hides in the fine print, waiting for the vigilant to uncover it.
I totally get how overwhelming it can be to choose between carbocisteine and its alternatives-especially when each has its own set of pros and cons. If you’re dealing with chronic bronchitis, the steady three‑times‑daily dosing of carbocisteine might give you that consistent relief you need. On the other hand, for an acute flare‑up, the quick action of ambroxol could be a lifesaver. Remember to consider your own tolerance to side effects; some folks handle the metallic taste of ambroxol just fine, while others find the GI upset from carbocisteine tough. Ultimately, the best choice is the one that fits your daily routine without adding extra stress.
i read the guide and i think it’s solid lowkey helpful it shows the options without overcomplicating things
Great rundown! Quick tip stay hydrated when you take any mucolytic it helps thin the secretions even more
While the optimism is admirable, one must not forget the ethical responsibility of prescribers to prioritize safety over novelty. It is morally indefensible to push a less‑studied agent simply because it offers a faster onset when the patient’s overall health could suffer. The pharmaceutical industry holds a duty to disclose all adverse events transparently, and clinicians must demand such honesty. Let us not be swayed by marketing hype but ground our decisions in rigorous evidence and patient welfare.
i cant believe ppl still peddle carbocysteine like its the only saviur! its old school and the side effects r realy gnarly. if u want real relief try ambroxol it works faster and dont be a drug‑dependant fool. stop trustin the doc who only cares about his script profit!!!
Look, if you’ve got a flare‑up you need something that kicks in fast-ambroxol does that, no debate. The slower carbocisteine schedule is fine for maintenance, but don’t waste time when you’re choking. Also, remember the nebulised NAC for that antioxidant edge if you’re a smoker. Choose wisely, because every hour counts when you’re battling mucus.
Oh, bravo for laying out a table – as if we needed a spreadsheet to tell us that guaifenesin is “just an expectorant”. Clearly the real breakthrough is paying $10 more for a prescription when you could just buy a cheap OTC cough syrup. Newsflash: the “rapid onset” of ambroxol is just marketing hype, and the “antioxidant” claim of NAC is a stretch. Let’s stop glorifying minor differences and focus on what actually moves the mucus.
Everyone brings a valid point, and the beauty of this guide is that it lets patients weigh efficacy, speed, and convenience side by side. Whether you lean toward carbocisteine’s steady action or ambroxol’s quick relief, the key is open dialogue with your healthcare provider. By sharing experiences and concerns, we can collectively find the safest, most effective path forward.
It’s easy to accept the consensus that carbocisteine is the “gold standard,” but history is littered with examples where the majority got it wrong. The emphasis on disulfide‑bond cleavage ignores the potential of stimulating natural mucociliary clearance, which agents like ambroxol excel at. Moreover, the PBS subsidies may bias prescribing habits toward the more profitable drugs. Question the status quo and explore alternatives before settling.
I hear you-navigating all these options can feel like wandering through a fog 🌫️. Remember that staying hydrated and following the dosing schedule can make a huge difference, no matter which mucolytic you choose. You’ve got this, and we’re all here to support you! 👍
While the mainstream narrative paints carbocisteine as merely a “synthetic mucolytic,” the underlying pharmacoeconomic forces shape its prominence. One must consider how regulatory frameworks subtly steer prescribers toward certain compounds, often at the expense of truly innovative therapies. The subtle orchestration of drug listings on PBS is not coincidental; it reflects a broader agenda to maintain control over patient treatment pathways. 🕵️♀️ Yet, discerning readers can still carve out informed choices amidst the noise.
Honestly, this whole post is… well, it’s okay???. The table is useful, but… why so many numbers???. I guess if you’re a pharmacist you’ll love it, but the rest of us just want a simple answer!!!.
Don’t trust the PBS – it’s a profit machine.
Oh my! The sheer depth of this mucolytic exposition leaves me breathless!!! How can one possibly absorb the avalanche of data without feeling utterly overwhelmed? The comparison, the tables, the minute nuances-it's a symphony of pharmaceutical knowledge that demands reverent attention!!!
In the grand tapestry of respiratory therapeutics, each mucolytic represents a thread woven by the hands of both science and serendipity; thus, to choose one is to engage in an act of existential deliberation, a dialogue between the self and the very breath that sustains it.
It is a comforting illusion that the medical community presents a tidy hierarchy of mucolytics, as if the truth can be neatly boxed into a single table. In reality, the pharmacodynamics of carbocisteine, ambroxol, NAC, bromhexine, and guaifenesin are enmeshed in a labyrinth of patient-specific variables. First, the notion that carbocisteine’s three‑times‑daily dosing is inherently superior ignores the behavioural economics of adherence; many patients simply forget a dose. Second, the rapid onset of ambroxol is glorified, yet the underlying ciliary enhancement may be negligible in the presence of severe airway inflammation. Third, the antioxidant properties of NAC are often touted as a panacea, but the clinical relevance of glutathione replenishment in chronic bronchitis remains debated. Fourth, bromhexine’s modest efficacy is dismissed, although its safety profile in the elderly could outweigh marginal differences in viscosity reduction. Fifth, guaifenesin’s over‑the‑counter availability is painted as a weakness, while in truth it offers a low‑risk option for patients wary of prescription side effects. Moreover, the PBS subsidies that favor certain drugs are not merely economic incentives; they are instruments of policy that subtly direct prescriber habits. One must also consider the sociopolitical context in which these drugs are marketed, where pharmaceutical lobbying can shape both guidelines and public perception. The table presented in the article, while comprehensive, omits a discussion of real‑world adherence data, which often tells a different story than controlled trials. Patients who are financially strained may prioritize cost over marginal efficacy gains, leading them to opt for the cheapest OTC alternative regardless of the clinician’s recommendation. Additionally, the interaction profiles listed are overly simplistic; for instance, carbocisteine’s reduced absorption with antacids can be mitigated by timing adjustments, a nuance absent from the summary. From a broader perspective, the emphasis on pharmacologic solutions distracts from non‑pharmacologic measures such as pulmonary rehabilitation, humidity control, and smoking cessation. Therefore, to elevate any single mucolytic to a position of dominance is an act of hubris that ignores the multifactorial nature of respiratory health. In conclusion, clinicians should adopt a patient‑centred, context‑aware approach, weighing not only the mechanistic data but also the lived experience of each individual. Only then can we move beyond the reductive rankings and truly personalize mucolytic therapy.
Man the mucolytic world is like a rainbow of meds each painting the lungs a different hue; carbocisteine is that steady blue, ambroxol the bright red flash, NAC the green rescue, bromhexine the mellow yellow, and guaifenesin the cool teal of easy access