Most people think of loperamide as a simple fix for a bad stomach. You buy it at the pharmacy without a prescription, pop a couple of pills, and the diarrhea stops. It’s safe, right? Not always. What many don’t realize is that taking way more than the label says can turn this common medicine into a dangerous, even deadly, substance.
How Loperamide Works - And How It Can Go Wrong
Loperamide, sold under brands like Imodium A-D, is an opioid that works in your gut. At normal doses - 4 mg at first, then 2 mg after each loose stool, up to 8 mg a day - it slows down your intestines. It doesn’t cross into your brain because of a natural defense system called P-glycoprotein. That’s why it doesn’t make you high or cause the typical opioid side effects like drowsiness or euphoria.
But when someone takes 50 to 400 mg a day - sometimes even more - that defense breaks down. The drug floods into the bloodstream, crosses the blood-brain barrier, and starts acting like other opioids. People do this not for fun, but because they’re trying to manage opioid withdrawal. They’re desperate. They’ve heard loperamide is easy to get, doesn’t require a prescription, and might help with cramps, sweating, anxiety - all the awful symptoms of quitting heroin or painkillers.
Here’s the problem: loperamide doesn’t give you a strong high. So users keep taking more. And more. And more. What they don’t know is that each extra pill increases the risk of their heart stopping.
The Silent Killer: Heart Damage from Loperamide Abuse
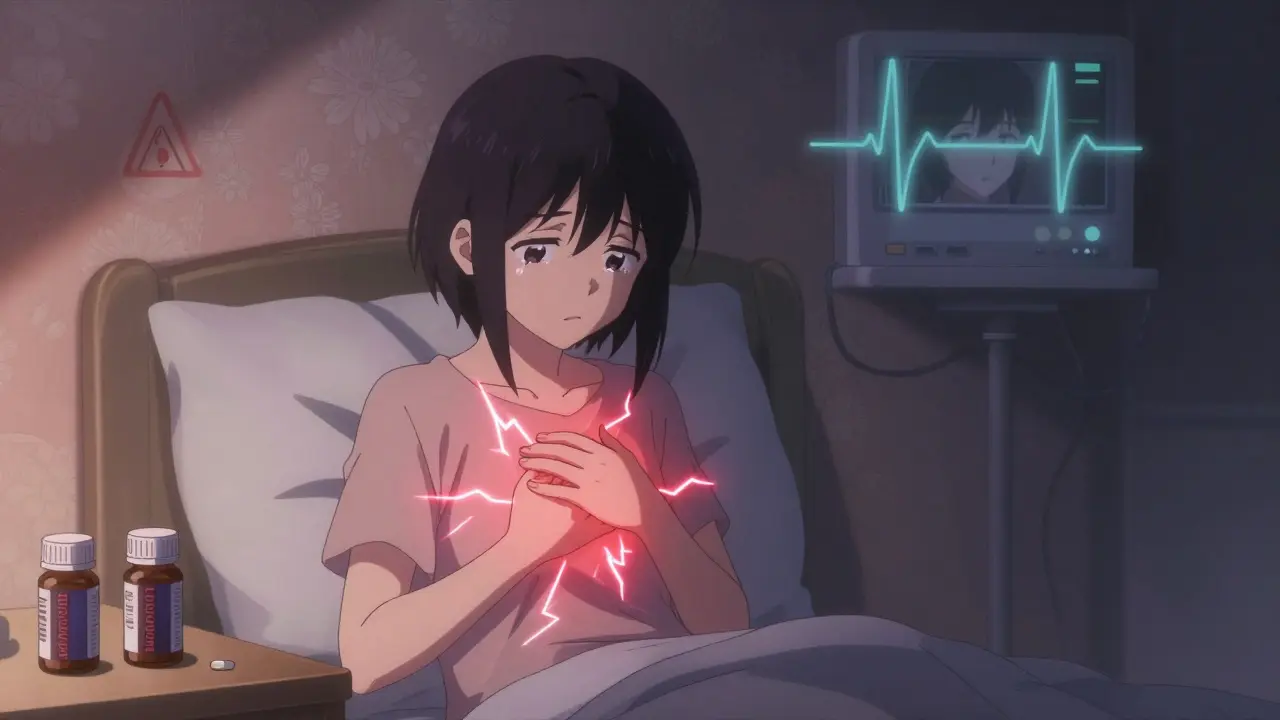
The biggest danger isn’t addiction - it’s cardiac arrest. At high doses, loperamide blocks important electrical channels in the heart, especially the hERG potassium channel. This causes the heart’s rhythm to go haywire. The ECG shows a dangerously long QT interval, sometimes a widened QRS complex. These changes can trigger a type of irregular heartbeat called torsades de pointes, which can spiral into sudden cardiac death.
The FDA reviewed 48 serious cases of heart problems linked to loperamide. More than half happened after 2010. In one case, a 32-year-old man took 80 mg a day (20 times the max recommended dose) to fight opioid withdrawal. He ended up in the ER with polymorphic ventricular tachycardia - his heart was fluttering uncontrollably. He survived, but barely.
Another case involved a person who took 30 mg daily. Their QTc (a measure of heart rhythm) was borderline at 436 ms. By the time they reached 100 mg, their QTc shot past 500 ms - a red flag for imminent danger. Even people who don’t have heart disease before are at risk. There’s no safe threshold for abuse. The damage builds up silently.
Warning Signs No One Talks About
Most people don’t recognize loperamide abuse until it’s too late. The signs aren’t always obvious. Here’s what to watch for:
- Heart palpitations - feeling like your heart is skipping, racing, or pounding
- Chest pain or pressure, especially if it comes out of nowhere
- Dizziness, fainting, or sudden collapse
- Nausea, vomiting, or extreme constipation - signs your gut has shut down
- Unexplained cardiac arrest in someone with a history of opioid use
Doctors often miss this. If a young, otherwise healthy person collapses with no known heart condition, loperamide abuse should be on the list. Standard drug tests don’t detect it. You need a specific blood test. And if someone’s been using it for weeks, the drug can stay in their system longer than expected, making the risk linger.

Why People Turn to Loperamide - And Why It’s a Trap
It’s not about getting high. It’s about survival. People with opioid use disorder are often stuck. They can’t afford or access methadone or buprenorphine. They don’t have insurance. They’re afraid of clinics. So they turn to what’s cheap, legal, and easy: loperamide.
Online forums like Reddit’s r/opioidrecovery are full of stories. One user wrote: “Tried 50 mg Imodium to help with withdrawal… wound up in ER with chest pains.” Another said, “I took 100 mg over two days. Felt like I was dying. My heart wouldn’t stop racing.” These aren’t outliers. The National Poison Data System recorded over 5,000 loperamide exposures in 2017 - up 91% since 2011. Nearly half were intentional misuse. And between 2011 and 2020, at least 17 people died from loperamide toxicity.
Some users even mix loperamide with other drugs to make it work faster - like quinidine, cimetidine, or diphenhydramine. These block the enzymes that break down loperamide, letting more of it reach the brain. It’s a deadly cocktail. One wrong combo, and the heart can’t recover.
What’s Being Done - And What’s Still Missing
The FDA issued a safety warning in 2016. Since then, manufacturers have changed packaging. Some products now come in single-dose blister packs if they contain more than 45 mg total. Sales dropped 12% between 2016 and 2020. But abuse didn’t stop - it just moved online. People now buy bulk bottles from international websites or use multiple prescriptions from different pharmacies.
Pharmacies have started limiting how many packages one person can buy. But that’s not enough. There’s no requirement for a prescription. No mandatory counseling. No system to flag high-volume buyers. And most importantly - most people still don’t know the risks.
Even SAMHSA and the American Academy of Family Physicians now warn: loperamide is not a safe substitute for opioid treatment. It doesn’t work like methadone or buprenorphine. It doesn’t have medical oversight. And it carries a hidden, deadly risk no one talks about until it’s too late.

What to Do If You or Someone You Know Is Using Loperamide to Manage Withdrawal
If you’re using loperamide to get through opioid withdrawal, stop. The risk isn’t worth it. You don’t need to suffer alone. There are safer, proven options:
- Call SAMHSA’s National Helpline at 1-800-662-HELP (4357). It’s free, confidential, and available 24/7.
- Ask your doctor about buprenorphine. It’s FDA-approved, effective, and safe when monitored.
- Find a local medication-assisted treatment (MAT) program. Many offer sliding-scale fees or free services.
- If you’ve taken more than 8 mg in a day and feel your heart racing, dizzy, or in pain - go to the ER. Tell them you took loperamide. Don’t wait.
Family members, friends, or caregivers should pay attention. If someone with a history of opioid use starts buying large amounts of Imodium, hoarding pills, or has unexplained chest pain - don’t ignore it. Ask. Push for help. This isn’t just about diarrhea anymore. It’s about saving lives.
Final Thought: Just Because It’s Over-the-Counter Doesn’t Mean It’s Safe
Medicines aren’t safe just because you can buy them without a prescription. Aspirin can cause bleeding. Acetaminophen can kill your liver. And loperamide? It can stop your heart - quietly, without warning, and often in people who think they’re being smart.
The system needs to do more. But until then, awareness is the best defense. If you’ve ever thought about using loperamide to get through withdrawal - know this: there are better, safer ways. And if you’re caring for someone who might be doing it - speak up. They might not realize how close they are to the edge.
Can you get high off loperamide?
Loperamide doesn’t produce a strong high like heroin or oxycodone. At abusive doses, some users report mild euphoria, sedation, or a sense of calm - but it’s weak and comes with serious side effects. Most people take huge amounts (100+ mg) just to feel anything, which puts them at extreme risk of heart failure. It’s not worth it.
How much loperamide is dangerous?
The maximum safe daily dose for over-the-counter use is 8 mg. Anything above 100 mg is considered abuse and carries serious cardiac risk. Doses of 200 mg or more have been linked to fatal arrhythmias. There’s no safe amount for recreational or withdrawal use.
Can naloxone reverse loperamide overdose?
Naloxone can reverse some of the central nervous system effects of loperamide - like sedation - but it does NOT fix the heart damage. The real danger - QT prolongation, torsades de pointes, cardiac arrest - won’t be reversed by naloxone. Immediate medical care, including cardiac monitoring and magnesium sulfate, is critical.
Is loperamide addictive?
Loperamide isn’t addictive in the traditional sense like heroin or cocaine. But people can develop a physical dependence, especially when using it daily to manage opioid withdrawal. Stopping suddenly can cause withdrawal symptoms like anxiety, sweating, and nausea - which can lead to more use. It’s a cycle, not a cure.
How do doctors test for loperamide abuse?
Standard urine drug screens don’t detect loperamide. Doctors need a specific blood test to measure loperamide levels. If someone presents with unexplained cardiac issues and a history of opioid use, clinicians should suspect loperamide abuse and request this test. ECG changes - especially prolonged QTc - are key indicators.
Are there safer alternatives to loperamide for opioid withdrawal?
Yes. Medications like buprenorphine and methadone are FDA-approved, medically supervised treatments for opioid withdrawal and addiction. They’re safer, more effective, and don’t carry the risk of sudden cardiac death. Support programs, counseling, and behavioral therapy also play a vital role. Loperamide is not a substitute - it’s a dangerous shortcut.
What to Do Next
If you’re using loperamide to cope with withdrawal, reach out. Call a helpline. Talk to a doctor. You don’t have to do this alone.
If you’re worried about someone else - a friend, family member, coworker - don’t wait for them to hit rock bottom. Ask them if they’re okay. Offer to help them find resources. That one conversation could save a life.
Loperamide isn’t the villain. It’s a tool that’s being misused in a crisis. The solution isn’t to take it off the shelves - it’s to make sure people know the truth before they take that first extra pill.

Loperamide abuse is such a classic example of how capitalism turns medicine into a free-for-all. You can buy a cardiac toxin like it’s candy, while people who need real treatment are stuck in bureaucratic purgatory. The FDA warning in 2016? Too little, too late. And now they slap on blister packs like that’s some kind of moral victory. Pathetic.
Hey, I just want to say - if you’re reading this and you’re using loperamide to get through withdrawal, please know you’re not alone 💕 I’ve been there. It’s scary, it’s lonely, but there IS a way out. Call the SAMHSA helpline. Just one call. I did it. I’m here now. You can be too 🌻 You deserve peace, not a heart attack.
AMERICA IS DYING. People are popping Imodium like Skittles while the government sits on its hands. This isn’t just drug abuse - it’s the collapse of the moral fabric. We let corporations sell poison because it’s ‘legal’? That’s not freedom. That’s surrender. And if you think this is about diarrhea, you’re blind. This is about a nation that stopped caring. 💀🇺🇸
The pharmacokinetics of loperamide are well-documented: P-glycoprotein efflux saturation at supra-therapeutic doses leads to CNS penetration, resulting in hERG channel blockade. The QTc prolongation is dose-dependent and non-linear. Clinical correlation with torsades de pointes is statistically significant (p<0.001). The real issue is the absence of pharmacovigilance infrastructure in OTC markets. You cannot regulate stupidity.
wait so if someone takes like 150mg and their ecg shows a qtc of 500… is that like… immediately life threatening? or can they just chill and wait it out? i’m asking because my cousin did this and the er doc just said ‘don’t do it again’ and sent him home… that feels wrong??
Actually, Jeane, that’s exactly what’s wrong. A QTc >500 ms is an emergency. Naloxone won’t fix it. Magnesium sulfate is first-line. Cardiac monitoring for 24+ hours is mandatory. If the ER discharged him without telemetry, they committed malpractice. Also - he needs a toxicology screen for co-ingestants. Quinidine? Diphenhydramine? Those are force multipliers. He’s lucky he’s alive.
My brother went through this last year… he took 200 mg over three days trying to quit oxy. He woke up in the hospital with his heart doing the cha-cha. He didn’t even know it was dangerous. No one told him. And now? He’s in a MAT program. He’s got a job. He’s alive. I just want people to know - you don’t have to suffer like that. There’s help. Real help. Not a pharmacy aisle. Please - reach out. You’re worth it.
Wait - so you’re saying loperamide is dangerous… but methadone isn’t? Methadone is a Schedule II opioid that requires daily clinic visits and costs hundreds per month. Loperamide is $5 and available next to gum and batteries. Who’s really being irresponsible here? The person trying to survive - or the system that makes survival so damn hard? This isn’t about ‘abuse.’ It’s about neglect.
im sorry but i just dont get why people think this is okay? like… you know its bad but you do it anyway? its like eating bleach because you're thirsty? i dont get it
They’re not stupid. They’re targeted. Big Pharma knew. They knew people would use it this way. They didn’t change the packaging because they wanted the sales. They waited for the deaths. Then they made a press release. This is a profit-driven genocide. The FDA is complicit. The pharmacies are complicit. The doctors who dismiss it? Complicit. You think this is an accident? No. This is the system working exactly as designed.