What Are Gallstones, and Why Do They Happen?
Most people don’t think about their gallbladder until it hurts. That sudden, sharp pain under the right rib cage-often after a fatty meal-can be a gallstone attack. Gallstones are hard deposits that form inside the gallbladder, a small organ tucked under the liver that stores bile. About 10-15% of adults in the U.S. have them, and women are more likely to get them than men. In fact, 14.2 million of the 20.5 million Americans with gallstones are women.
There are two main types: cholesterol stones and pigment stones. About 80% of gallstones are made of cholesterol, which builds up when bile has too much of it or not enough bile salts to keep it dissolved. The other 20% are pigment stones, made mostly of bilirubin, a waste product from broken-down red blood cells. These are more common in people with liver disease, sickle cell anemia, or in Asian populations. Mixed stones, which have both, are also common.
Many people have gallstones and never know it. In fact, up to 80% of people with gallstones are asymptomatic. The American College of Gastroenterology says if you have no symptoms, you don’t need surgery. The risk of a serious complication in a year is only 1-2%. But if you start having pain, nausea, or vomiting after meals, especially fatty ones, that’s when things get serious.
When Gallstones Cause Trouble: Cholecystitis and Cholangitis
A gallstone blocking the cystic duct-the tube that connects the gallbladder to the bile duct-can cause acute cholecystitis. That’s inflammation of the gallbladder. It’s the most common complication, happening in about 90% of cases where a stone gets stuck. Symptoms include severe pain in the upper right abdomen, fever, nausea, and sometimes jaundice. Hospitalization is often needed, and surgery to remove the gallbladder is usually the next step.
But if the stone moves and blocks the common bile duct or the ampulla of Vater, things get much more dangerous. That’s when cholangitis happens. This is an infection of the bile ducts, and it can turn deadly fast. The classic signs, called Charcot’s triad, are right upper quadrant pain, fever, and jaundice. If you add low blood pressure and confusion, that’s Reynolds’ pentad-and it means you’re in septic shock. About 85% of cholangitis patients have fever, 70% have pain, and 60-70% turn yellow. Without quick treatment, the infection can spread, leading to organ failure.
People with diabetes, cirrhosis, or who’ve had prior biliary surgery are at higher risk. And while cholecystitis is common, cholangitis is rarer-only 10-15% of gallstone complications-but far more serious. It’s why doctors don’t wait when a stone might be stuck in the bile duct.
ERCP: The Procedure That Fixes Blocked Bile Ducts
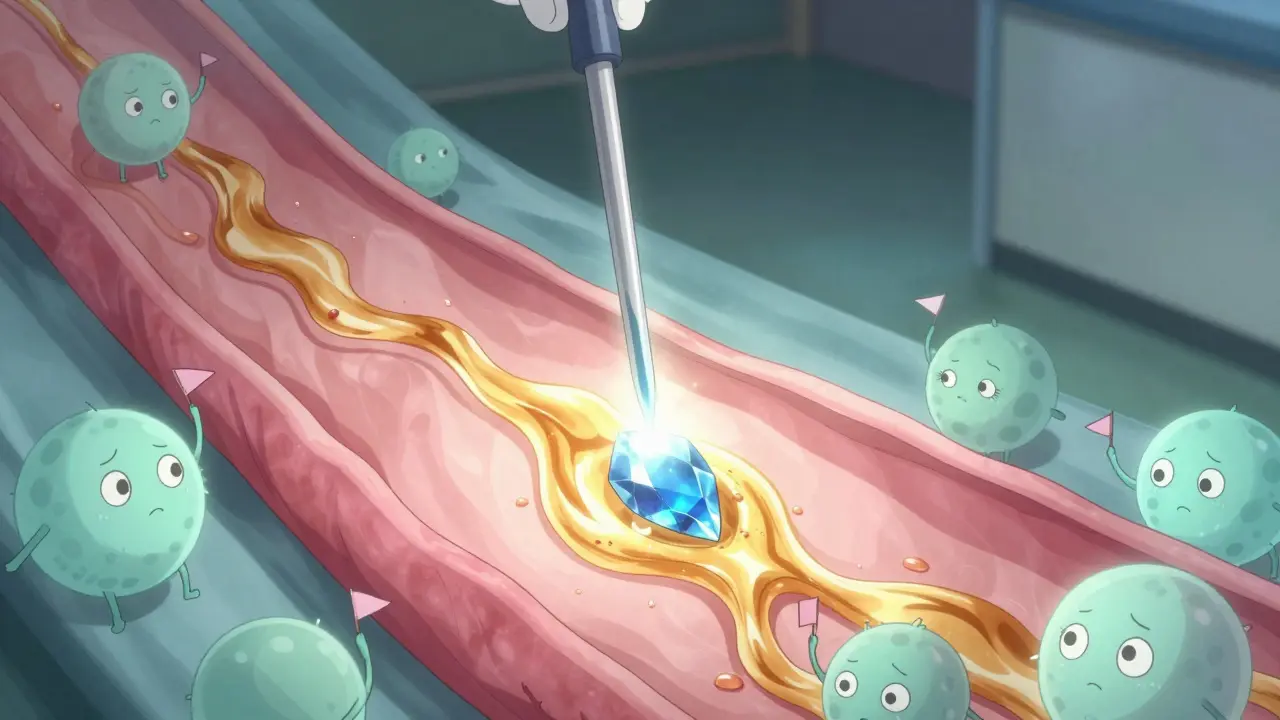
When a stone is stuck in the bile duct, ERCP-Endoscopic Retrograde Cholangiopancreatography-is often the go-to fix. It’s not just a diagnostic tool; it’s a treatment. Developed in the late 1960s and refined since the 1990s, ERCP lets doctors see the bile and pancreatic ducts using a thin, flexible tube passed through the mouth, down the throat, and into the small intestine. A tiny camera and tools go through the scope to find and remove stones.
The procedure involves cutting the muscle around the duct opening (sphincterotomy) to let stones pass or using a basket or balloon to pull them out. Success rates in experienced hands are over 90%. Most patients feel better within hours. One Reddit user wrote, “ERCP recovery was surprisingly quick-I was back to desk work in 48 hours.”
But ERCP isn’t risk-free. About 3-10% of people develop post-ERCP pancreatitis, where the pancreas gets inflamed. That’s the most common complication. Risk goes up if you have Sphincter of Oddi dysfunction, or if the procedure is done by someone with low volume. Centers that do more than 100 ERCPs a year have 20% fewer complications than those doing fewer than 50. That’s why it’s best done in high-volume centers.
Doctors now use MRCP (Magnetic Resonance Cholangiopancreatography) first to confirm a stone is in the bile duct. MRCP is non-invasive, has 95% sensitivity, and doesn’t carry the risks of ERCP. Only if a stone is confirmed and needs removal does ERCP follow. The American Society for Gastrointestinal Endoscopy says ERCP should never be used just to look-only to treat.
When Surgery Is the Answer: Laparoscopic Cholecystectomy
If you have symptomatic gallstones, removing the gallbladder is the most effective long-term solution. Laparoscopic cholecystectomy is now the gold standard. It’s done with small incisions, a camera, and tiny tools. Patients go home the same day or the next. Recovery takes about 7-10 days, compared to 4-6 weeks with open surgery.
Over 90% of gallbladder removals in the U.S. are now laparoscopic. The procedure is safe, with patient satisfaction ratings averaging 4.5 out of 5. About 87% report major symptom relief within 30 days. But it’s not perfect. Around 12% of patients still have ongoing abdominal pain, called post-cholecystectomy syndrome. Some get diarrhea because bile flows directly into the intestine without being stored. That’s usually temporary, but a few need medication like loperamide for months.
Here’s the problem: about 20% of the 600,000 cholecystectomies done each year are on people who barely had symptoms. Guidelines say only those with clear, recurrent pain should get surgery. Too many are still being operated on unnecessarily.
What Doesn’t Work-And Why
There are treatments people hear about that don’t hold up. Ursodeoxycholic acid (UDCA) can dissolve small cholesterol stones under 15mm, but only in 30-40% of cases, and it takes 6-12 months. It doesn’t work on pigment stones at all. That means only 10-15% of people with gallstones are even candidates.
Shock wave lithotripsy, which breaks stones apart with sound waves, was tried in the 1990s. But stones often came back. Studies show 50% of patients had new stones within five years. It’s rarely used now.
And while some people swear by gallbladder cleanses or herbal remedies, there’s zero scientific proof they work. In fact, some have caused serious harm. The only proven methods are surgery, ERCP, and, in rare cases, medication.
Who’s at Risk-and How to Lower It
Some risks you can’t change. Age is one. By age 60, 25% of people have gallstones. Being female is another-women are 2.1 times more likely than men. Native Americans, especially Pima Indians, have the highest rates in the world, with up to 64% affected.
But many risks are lifestyle-based. Obesity increases your risk two to three times. Rapid weight loss-like from crash diets or bariatric surgery-is a major trigger. Losing more than 1.5 kg per week can cause bile to become supersaturated with cholesterol, leading to stone formation. Diabetes doubles or triples your risk. Cirrhosis increases it four to six times.
Prevention isn’t about avoiding fat. It’s about avoiding extremes. Eat regular meals. Don’t skip breakfast. Lose weight slowly. Keep your blood sugar under control. These steps don’t guarantee you won’t get stones, but they help.

What Happens After ERCP or Surgery
After ERCP, you’ll be monitored for pancreatitis. You might have a sore throat from the scope-it usually fades in a few days. You’ll be told to eat lightly for the rest of the day. Most people resume normal activities in 24-48 hours.
After gallbladder removal, you’ll be on a low-fat diet for 2-4 weeks. Fat digestion is harder without the gallbladder to store and release bile on demand. After six weeks, 75% of people can eat normally again. But some will have loose stools, especially after fatty meals. That’s normal. It often improves over time. If it doesn’t, talk to your doctor about bile acid binders.
Follow-up isn’t always needed unless symptoms return. But if you had ERCP to remove a bile duct stone, your doctor will check that all stones are gone. Only 30-40% of patients get both the ERCP and cholecystectomy done at the same time. That’s a missed opportunity. Doing both together cuts down on extra procedures, hospital stays, and costs.
What’s New in 2026
Technology keeps improving. In 2023, the FDA approved a new duodenoscope with a fully disposable elevator mechanism. That’s important-previous designs were linked to 112 outbreaks of drug-resistant infections between 2013 and 2018. Now, the part that touches inside the duct is single-use, reducing contamination risk.
Intraductal ultrasonography (IDUS) is also becoming more common. It uses a tiny ultrasound probe passed through the ERCP scope to see stones smaller than 5mm that standard imaging misses. Sensitivity jumps from 75% to 92%.
Researchers are working on new drugs to dissolve pigment stones, which currently have no good medical treatment. The American Gastroenterological Association’s 2023 roadmap lists this as a top priority.
Telehealth is helping too. Post-ERCP check-ins via video call have cut 30-day readmissions by 18% in pilot programs. That’s huge for patient safety and healthcare costs.
Final Thoughts
Gallbladder and biliary disease is common, but it’s not always obvious. Gallstones are often silent. Cholangitis is not. ERCP saves lives-but it’s not a first step. Surgery removes the problem-but only if it’s truly needed.
The key is knowing when to act. If you have pain, jaundice, or fever after a gallbladder attack, don’t wait. If you have stones but no symptoms, don’t rush to surgery. Ask your doctor: Is this stone causing my pain? Is it blocking my bile duct? Do I need ERCP now, or can I wait for an ultrasound and MRCP first?
There’s no one-size-fits-all. But with the right tests, the right timing, and the right team, most people get back to normal without long-term problems.


I had a gallstone attack last year. Felt like someone was stabbing me with a hot fork. Went to the ER, they did an ultrasound, found the stone, and I had my gallbladder out in 48 hours. Best decision I ever made. No more scary meals after tacos.
The data presented in this post is statistically sound, though it fails to account for regional disparities in healthcare access. The 1-2% annual complication rate assumes timely diagnosis, which is not universally achievable in underserved populations.
Funny how people think ERCP is some kind of magic wand. I had mine done last year. Yeah, the stone was gone. Then I spent six weeks with diarrhea that made me hate my own intestines. And the pancreatitis scare? Not fun. Surgery’s not perfect, but at least you know what you’re getting.
The gallbladder, as an organ, functions as a reservoir of bile, thereby facilitating the emulsification of dietary lipids in the duodenum. Its removal, while ostensibly resolving symptomatic cholelithiasis, introduces a state of continuous biliary flux, which may be physiologically incongruent with ancestral metabolic patterns.
You know what they don’t tell you? Gallstones are caused by fluoride in the water. The FDA knows it. Hospitals know it. That’s why they push surgery - it’s more profitable than fixing the water supply. I took apple cider vinegar and mine dissolved in 3 weeks. No surgery. No ERCP. Just truth.
In India, we see more pigment stones because of high rates of malaria and hemolytic disorders. ERCP is common here, but many still go to Ayurvedic practitioners first. Some herbal mixtures help with bile flow, but they don’t dissolve stones. Surgery is still the only real fix when it gets bad.
I’m just glad I didn’t wait. I had silent stones for years. One day I ate a burrito and thought I was dying. Turned out I was. Now I eat like a normal human again. No regrets. Just grateful.
This post is dangerously misleading. They say 80% of people with gallstones are asymptomatic - so why are we doing 600,000 surgeries a year? Because doctors are scared of lawsuits. Because insurance wants quick fixes. Because patients are too lazy to change their diet. This isn’t medicine. It’s industrialized fear.
I’m a nurse in a rural clinic. We don’t have MRCP machines. We don’t have high-volume ERCP centers. We have ultrasound and our gut. If someone has pain, fever, jaundice - we don’t wait for perfect imaging. We get them to a city hospital. Sometimes that’s the difference between life and death.
Post-ERCP pancreatitis remains a significant iatrogenic risk, with incidence inversely correlated with procedural volume. Centers performing fewer than 50 ERCPs annually demonstrate a 20% higher complication rate, per ASGE guidelines. MRCP should be the initial diagnostic modality in all non-emergent cases.
I know it sounds scary but honestly? After the surgery I felt like a new person. No more hiding from pizza. No more waking up in sweat because I ate something fatty. I used to think I was just bad at eating. Turns out I just had a broken organ. Now I eat everything and I’m happy. Seriously, if you’re on the fence - just do it. You’ll thank yourself.
My mom had ERCP and then cholecystectomy the same week. It was a mess but worth it. She was in pain for years and no one believed her. Now she hikes, cooks, travels. Don’t let anyone tell you it’s not worth it. You’re not weak for needing help. You’re smart.
Okay but what if you’re one of those people who gets diarrhea after surgery but also has IBS? And your doctor says it’s normal but you’re still having 8 bowel movements a day? And your insurance won’t cover bile acid binders because they say it’s ‘not medically necessary’? What then? I’ve been on loperamide for 2 years. I’m not ‘adjusting’. I’m surviving.
I’ve had 3 ERCPs. 2 gallbladder surgeries. 1 failed attempt at dissolving stones with pills. I’ve been in the hospital so many times my nurses know my coffee order. I’ve cried in waiting rooms. I’ve screamed in recovery. I’ve lost jobs because of this. And now some guy on Reddit says ‘just don’t eat fat’? Like I didn’t try that before I lost my liver function? Don’t talk to me about prevention. Talk to me about real help.
The evolution of biliary care reflects a broader shift toward evidence-based, patient-centered intervention. While technological advancements such as disposable duodenoscopes and IDUS have mitigated infectious risk and improved diagnostic precision, the ethical imperative remains: prioritize necessity over convenience, and patient outcomes over procedural volume.