Statins and ALS: What the Research Shows About Cholesterol Drugs and Neurodegeneration
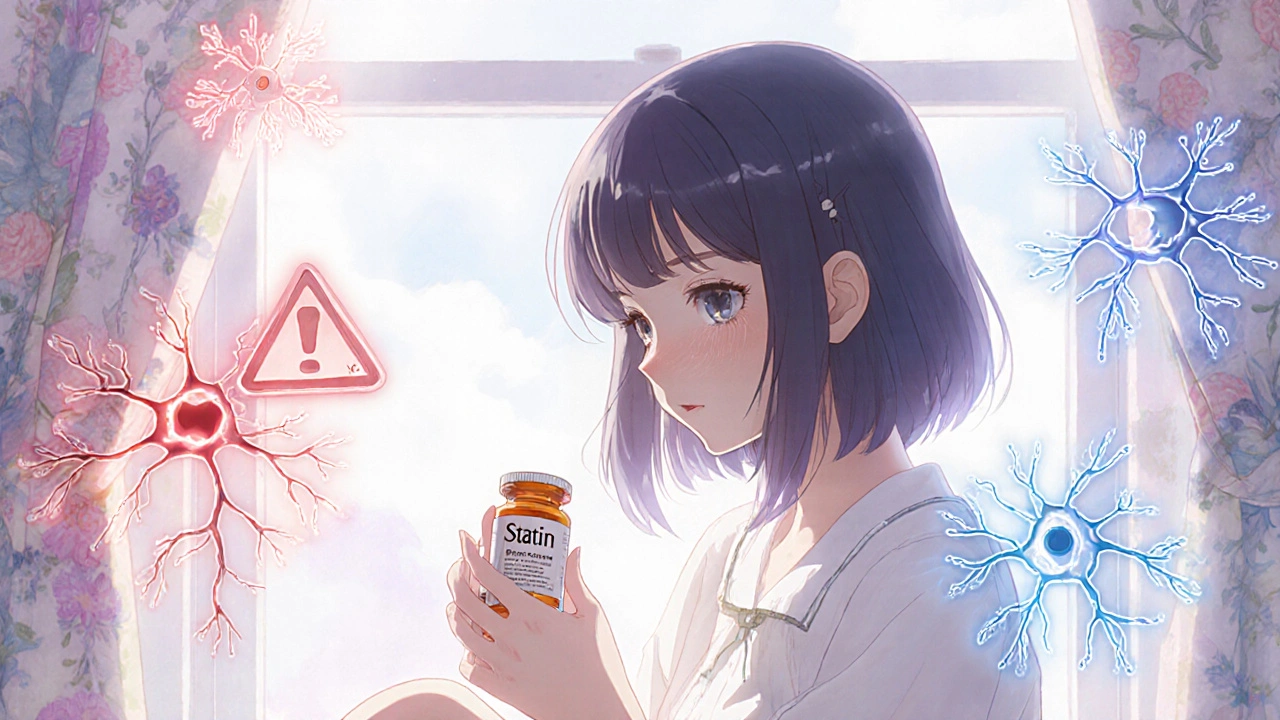
When you take a statin, a class of drugs used to lower LDL cholesterol and reduce heart attack risk. Also known as HMG-CoA reductase inhibitors, they're among the most prescribed medications in the world. But for some people, especially those with family history of neurological conditions, a quiet question lingers: could these drugs affect the nervous system in unexpected ways? Specifically, does taking a statin, a cholesterol-lowering drug commonly used to prevent cardiovascular disease raise the risk of ALS, a progressive neurodegenerative disease that destroys motor neurons, leading to muscle weakness and paralysis. Also known as Lou Gehrig's disease, it affects about 5,000 Americans each year?
The short answer? No clear link has been proven. Large population studies, including one published in Neurology tracking over 1.2 million people, found no increase in ALS diagnosis among statin users compared to non-users. In fact, some research suggests statins might even have a small protective effect—possibly by reducing inflammation or improving blood flow to nerves. But here’s the twist: a handful of case reports have described ALS-like symptoms appearing shortly after starting statins, especially in older adults with pre-existing nerve issues. These aren’t proof of cause, but they’re enough to make doctors pause and ask: is this a coincidence, or a rare reaction? The FDA has noted these reports but hasn’t changed labeling, because the evidence doesn’t support a widespread risk. What’s more important is that statins are prescribed for very real, life-saving reasons—heart disease kills far more people than ALS ever will.
So what should you do if you’re on a statin and worried about ALS? First, don’t stop taking it without talking to your doctor. The benefits for most people far outweigh any unproven risk. Second, pay attention to new symptoms: unexplained muscle weakness, trouble climbing stairs, slurred speech, or frequent falls aren’t normal aging—they’re red flags. If you notice them, get checked. Third, know your family history. ALS is rare, but if someone in your immediate family had it, discuss genetic testing with a neurologist. And remember: many factors influence ALS risk—age, smoking, military service, and even intense physical activity—none of which are tied to statins. The real story here isn’t about drugs causing disease. It’s about how medicine tries to untangle complex, rare events from the noise of everyday health. Below, you’ll find real patient stories, expert analyses, and studies that dig deeper into what we know, what we don’t, and how to make smart choices about your health.
Statins and ALS: What the Latest Science Really Says
Statins and ALS: What the science says. No proven link between statins and ALS. Long-term use may even reduce risk. Don't stop statins without medical advice.
- Drug Information (71)
- Health and Wellness (59)
- Pharmacy Information (25)
- Medical Conditions (24)
- Supplements (4)
- Diabetes (4)
- Travel Health (3)
- Mental Health (3)
- Heart Health (2)
- Parenting (2)
-
Assistive Technology for ADHD Students: Practical Tools and Tips
29 Sep 2025 -
The Role of Palliative Care in Mycosis Fungoides Treatment
21 Jul 2023 -
The Role of Genetics in Gouty Arthritis: Are You at Risk?
2 Jun 2023 -
Why Savin Tops is the Only Dietary Supplement You'll Ever Need for Weight Loss
1 Jul 2023 -
How to Choose OTC Eye Drops for Allergies, Dryness, and Redness
2 Dec 2025

23.11.25
Alistair Mukondiwa
11