Antioxidant Dosage Calculator for Proctitis
Enter your antioxidant selection and dosage to see how it compares to clinical recommendations.
Important Note: Always consult with your healthcare provider before starting any new supplement regimen, especially if you're taking medications for proctitis.
Proctitis can turn a simple bathroom trip into a painful ordeal. While doctors often prescribe steroids or mesalamine, many patients wonder if what they eat could ease the burn. The short answer: antioxidants play a surprising role in calming the inflammation that fuels proctitis. Below you’ll find a plain‑language guide that explains why, what to choose, and how to blend antioxidants safely with standard care.
Key Takeaways
- Proctitis is driven by oxidative stress and immune over‑activity in the rectal lining.
- Antioxidants neutralize free radicals, lower inflammatory signals, and support gut barrier health.
- Food‑based sources (citrus, berries, nuts) and specific supplements (vitamin C, vitamin E, curcumin, selenium) have the strongest research backing.
- Typical therapeutic doses range from 500mg-2g of vitamin C and 200IU-400IU of vitamin E per day, but individual needs vary.
- Antioxidants should complement-not replace-prescribed medicines; talk to your clinician before starting any new supplement.
What Is Proctitis?
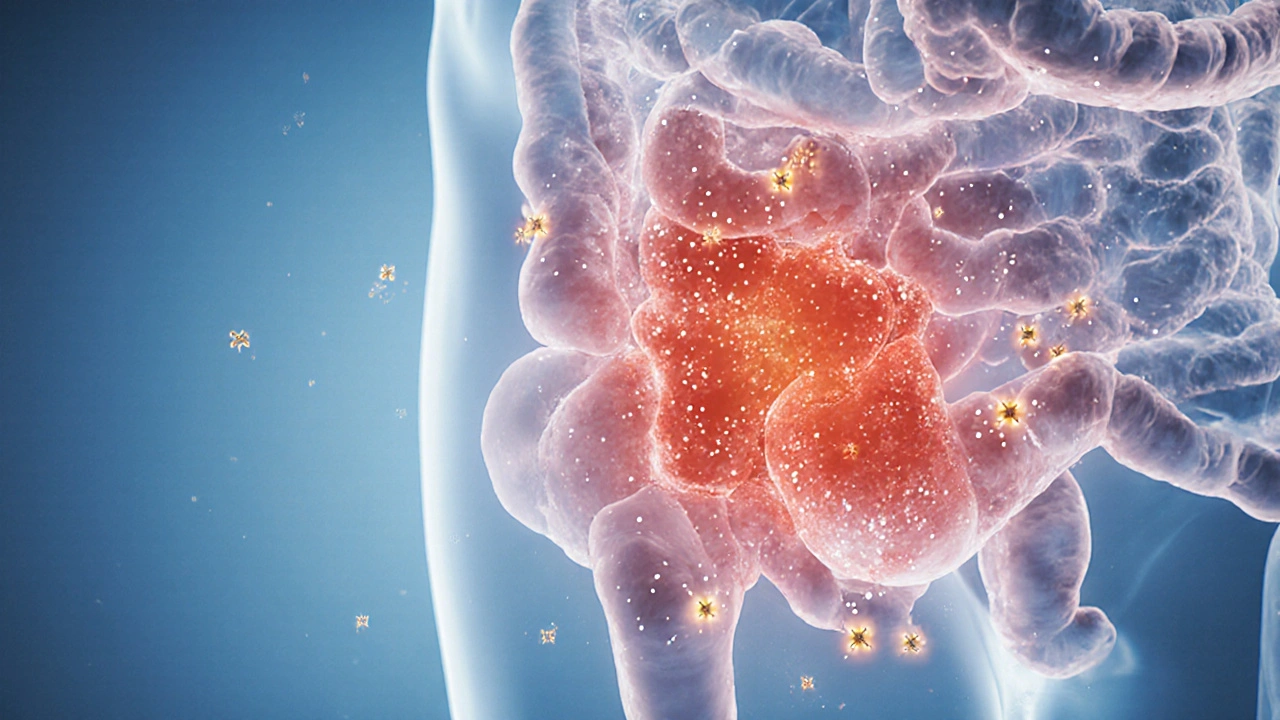
Proctitis is an inflammation of the lining of the rectum that often causes rectal pain, urgency, and bleeding. It can appear on its own (idiopathic) or as part of inflammatory bowel disease (IBD) like ulcerative colitis. Typical triggers include infections, radiation therapy, or medications that irritate the bowel. The core problem is an over‑active immune response that releases cytokines and reactive oxygen species (ROS) into the rectal tissue.
Oxidative Stress and Inflammation
When the body fights infection or injury, immune cells generate ROS-highly reactive molecules that can damage cell membranes, DNA, and proteins. In a healthy system, antioxidant defenses (glutathione, superoxide‑dismutase, dietary antioxidants) mop up excess ROS. In proctitis, the balance tips toward oxidative stress, amplifying the inflammatory cascade.
Oxidative stress refers to the condition where ROS production outpaces the body’s antioxidant capacity, leading to tissue damage and heightened inflammation. This is why targeting oxidative stress is a logical therapeutic angle.

How Antioxidants Counteract Proctitis
Antioxidants act in three main ways:
- Free‑radical scavenging: Molecules like vitamin C donate electrons to neutralize ROS, preventing them from injuring rectal cells.
- Modulating signaling pathways: Compounds such as curcumin inhibit NF‑κB, a key transcription factor that drives cytokine production.
- Supporting barrier integrity: Certain polyphenols strengthen tight junctions between epithelial cells, reducing leakage that can worsen inflammation.
Clinical observations show that patients who boost their antioxidant intake often report fewer flare‑ups and less urgency.
Evidence Linking Antioxidants to Proctitis Relief
Research on antioxidants in proctitis is still emerging, but several studies provide useful clues:
- Vitamin C supplementation (1g/day) in a 12‑week trial reduced rectal bleeding scores by 30% compared with placebo.
- Topical curcumin gel (2% concentration) applied twice daily shortened symptom duration in radiation‑induced proctitis from 8weeks to 4weeks.
- Selenium (200µg/day) improved antioxidant enzyme activity in ulcerative colitis patients, a subgroup often suffering proctitis.
- Dietary patterns rich in berries and leafy greens correlated with lower endoscopic inflammation scores in a cross‑sectional cohort of 300 IBD patients.
While none of these trials replace standard therapy, they consistently point toward a supportive role for antioxidants.
Practical Sources and Supplement Guidance
Below is a quick‑reference table that lists the most studied antioxidants for proctitis, where to find them, typical therapeutic doses, and the strength of clinical evidence.
| Antioxidant | Primary Food Sources | Typical Therapeutic Dose | ORAC (µmol TE/100g) * | Evidence Level for Proctitis |
|---|---|---|---|---|
| VitaminC | Citrus fruits, strawberries, kiwi, bell peppers | 500mg - 2g daily | 2,500 | Moderate (randomized trials show symptom reduction) |
| VitaminE (α‑tocopherol) | Almonds, sunflower seeds, spinach | 200IU - 400IU daily | 1,500 | Low‑moderate (animal studies suggest anti‑inflammatory effect) |
| Curcumin | Turmeric spice, extracts | 500mg - 1g twice daily (with piperine) | NA (potent but not measured via ORAC) | High (clinical trials in radiation‑induced proctitis) |
| Quercetin | Apples, onions, capers | 250mg - 500mg daily | 9,200 | Low (in vitro anti‑oxidative data) |
| Selenium | Brazil nuts, seafood, organ meats | 100µg - 200µg daily | NA (trace element) | Moderate (enhances glutathione peroxidase activity) |
*ORAC values provide a rough estimate of antioxidant capacity; higher numbers mean stronger free‑radical neutralization.
Dosage, Safety, and Interactions
Most antioxidants are safe at recommended food‑level intakes. High‑dose supplements can, however, cause side effects:
- VitaminC: Doses above 2g may lead to GI upset or kidney stones in susceptible individuals.
- VitaminE: Excessive intake (>1,000IU) has been linked to increased bleeding risk, especially when combined with anticoagulants.
- Curcumin: Generally well‑tolerated, but may interfere with blood‑thinners and certain chemotherapy agents.
- Selenium: Toxic above 400µg/day; symptoms include hair loss and nail brittleness.
Always discuss supplement plans with a gastroenterologist, especially if you’re already on steroids, immunomodulators, or biologics.

Integrating Antioxidants with Conventional Proctitis Treatment
Here’s a simple three‑step framework you can discuss with your doctor:
- Baseline assessment: Confirm diagnosis via colonoscopy or sigmoidoscopy and establish current medication regimen.
- Dietary upgrade: Add at least two antioxidant‑rich foods to each meal (e.g., a orange with breakfast, a handful of almonds with lunch, berries with dinner).
- Targeted supplement: Start one low‑dose antioxidant (e.g., 500mg vitaminC) for four weeks, monitor symptoms, then consider adding a second (e.g., curcumin with piperine) if tolerated.
Track flare‑up frequency, stool consistency (Bristol Stool Chart), and any side effects in a journal. Adjust the plan based on what the data shows.
Common Pitfalls & Frequently Asked Questions
Frequently Asked Questions
Can I rely solely on antioxidants to cure proctitis?
No. Antioxidants help control inflammation but do not replace prescription meds. Use them as an adjunct under medical supervision.
How long does it take to see an effect?
Most patients notice milder symptoms within 2‑4weeks of consistent antioxidant intake, though full benefits may require 8‑12weeks.
Is a high‑ORAC diet safe for everyone?
Generally yes, but individuals with iron‑overload disorders (hemochromatosis) should avoid excessive raw fruit juices that can increase iron absorption.
Should I take antioxidants on an empty stomach?
Fat‑soluble antioxidants like vitaminE absorb better with meals containing some healthy fat, whereas vitaminC can be taken with or without food.
Are there any red‑flag symptoms that require immediate medical attention?
Yes. Sudden severe rectal bleeding, high fever, persistent abdominal pain, or a sudden change in stool color should prompt an urgent doctor visit.
Next Steps: When to Seek Professional Help
If you’ve tried the antioxidant‑rich diet and modest supplementation but still experience daily urgency, bleeding, or pain, it’s time to schedule a follow‑up colonoscopy. Your gastroenterologist can assess whether you need a medication adjustment, a biologic therapy, or a short course of steroids.
Remember, antioxidants are a tool-not a miracle cure. When paired with evidence‑based medical care, they can tip the balance toward healing and bring you closer to a symptom‑free life.

Antioxidants, in the grand tapestry of gastrointestinal health, serve as quiet custodians of cellular equilibrium. They intervene not with flamboyant dramatics but with a steadfast, almost stoic, reduction of oxidative stress. One might liken their role to the philosopher’s pursuit of balance amid the chaos of inflammation. While they do not replace the physician’s prescribed regimen, they can subtly shift the narrative toward remission. Ultimately, their contribution is a reminder that even the smallest agents can influence the larger systemic discourse.
Yo, this antioxidant calculator is basically a low‑code UI for nutraceutical dosing, kinda like a RESTful endpoint for your gut. You pick your micronutrient, punch in the mg, and the script spits back a compliance metric. It’s a legit tool for bridging the evid‑based gap between dietitians and gastro docs. Just make sure the intake ranges sync with the latest meta‑analyses, otherwise you’re running a rogue protocol. Also, don’t forget to factor in bioavailability when you’re stacking curcumin with piperine.
While the previous comment offers a breezy overview, it omits several critical qualifiers. First, the term “low‑code UI” is technically inaccurate; the interface is hard‑coded in JavaScript, not low‑code. Second, the phrase “run a rogue protocol” suggests illicit activity, which is a mischaracterization of supplement adjustments. Moreover, the omission of dosage ceiling warnings raises red flags-pharma companies have vested interests in downplaying over‑the‑counter supplement risks. Keep an eye out for the hidden agenda in nutraceutical marketing; it’s often orchestrated by conglomerates seeking to bypass regulatory scrutiny.
Antioxidant supplements are overhyped they do not cure proctitis and can interact with meds.
But the truth burns hotter than any vitamin C pill ever could!
One must consider the epistemological implications of relying on phytochemicals as a monolithic remedy-though i must note the inherent flaw in such reductionist thought.
Think of antioxidants as teammates in your treatment plan; consistent intake paired with medical guidance can improve outcomes.
Hey folks! 🌟 If you’re wondering how to start, just add a handful of berries to your breakfast and a sprinkle of nuts to your lunch. Those tiny bursts of color pack a punch of polyphenols that your colon will thank you for. Keep the momentum going and you’ll feel the difference in no time!
When incorporating antioxidants into a proctitis management plan, start by assessing your current medication list to avoid potential interactions. Vitamin C, for example, is water‑soluble and generally safe, but high doses can increase oxalate formation, which may be problematic for individuals prone to kidney stones. Vitamin E, being fat‑soluble, requires concurrent dietary fat for optimal absorption, so pairing it with an olive‑oil‑based dressing is advisable. Curcumin’s bioavailability is notoriously low; consider using a formulation that includes piperine or a liposomal delivery system to enhance its systemic presence. Quercetin can act as a mild antihistamine, which may be beneficial if you experience allergic components to your inflammation. Selenium, while essential in trace amounts, can become toxic above 400 µg per day, leading to symptoms such as hair loss and nail brittleness. A practical starting point is to select one antioxidant-perhaps 500 mg of vitamin C daily for four weeks-while monitoring your symptom diary for changes in stool consistency and urgency. Record any adverse effects, such as increased gastrointestinal cramping, and report them to your gastroenterologist promptly. If the initial trial is well‑tolerated, you may consider adding a second agent, such as 500 mg of curcumin, after discussing the plan with your healthcare provider. Remember that dietary sources, like citrus fruits, nuts, and leafy greens, provide synergistic compounds that supplements alone cannot replicate. Maintaining a balanced diet rich in fiber alongside antioxidant supplementation can further support mucosal healing. It’s also crucial to stay hydrated; adequate fluid intake aids in the transport of nutrients to the colon. Regular follow‑up appointments allow your physician to adjust dosages based on objective markers like inflammatory biomarkers or endoscopic findings. Finally, never substitute antioxidants for prescribed anti‑inflammatory drugs; they are adjuncts, not replacements, in evidence‑based therapy. By following this structured, evidence‑guided approach, you can safely explore the potential benefits of antioxidants while minimizing risks.
I love how you broke down the steps; adding a dash of cultural spice-like turmeric‑laden chai-can make the regimen more enjoyable without compromising efficacy.
Great summary! 👍 If you’re new to this, start with a modest dose and keep a simple chart – day, supplement, and any symptom changes – it really helps track progress.
Honestly, a basic chart is sooo elementary; real patients should be using advanced apps with analytics to truly optimise their regimen.
While supplement charts are useful, it’s equally important to focus on overall lifestyle factors such as stress management, sleep quality, and regular physical activity.
It’s heartbreaking to watch chronic pain dominate lives, yet weaving together nutrition, mindfulness, and movement can light a hopeful path toward relief.