Warfarin-Antibiotic Interaction Checker
When you're on warfarin, even a simple course of antibiotics can throw your blood thinning off balance - and sometimes, dangerously so. It’s not about fear. It’s about awareness. Warfarin has been used for over 70 years to prevent strokes, clots, and dangerous blood thickening, especially in people with mechanical heart valves or certain types of atrial fibrillation. But it’s not a medication you can take lightly. And when antibiotics enter the picture, things get complicated fast.
Why Antibiotics and Warfarin Don’t Mix Easily
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But here’s the catch: about 10-15% of your vitamin K comes from bacteria in your gut. When you take antibiotics - especially broad-spectrum ones - you kill off those helpful bacteria. Less vitamin K means your blood thins more than expected. That’s one reason your INR (a measure of how long it takes your blood to clot) can spike without warning.
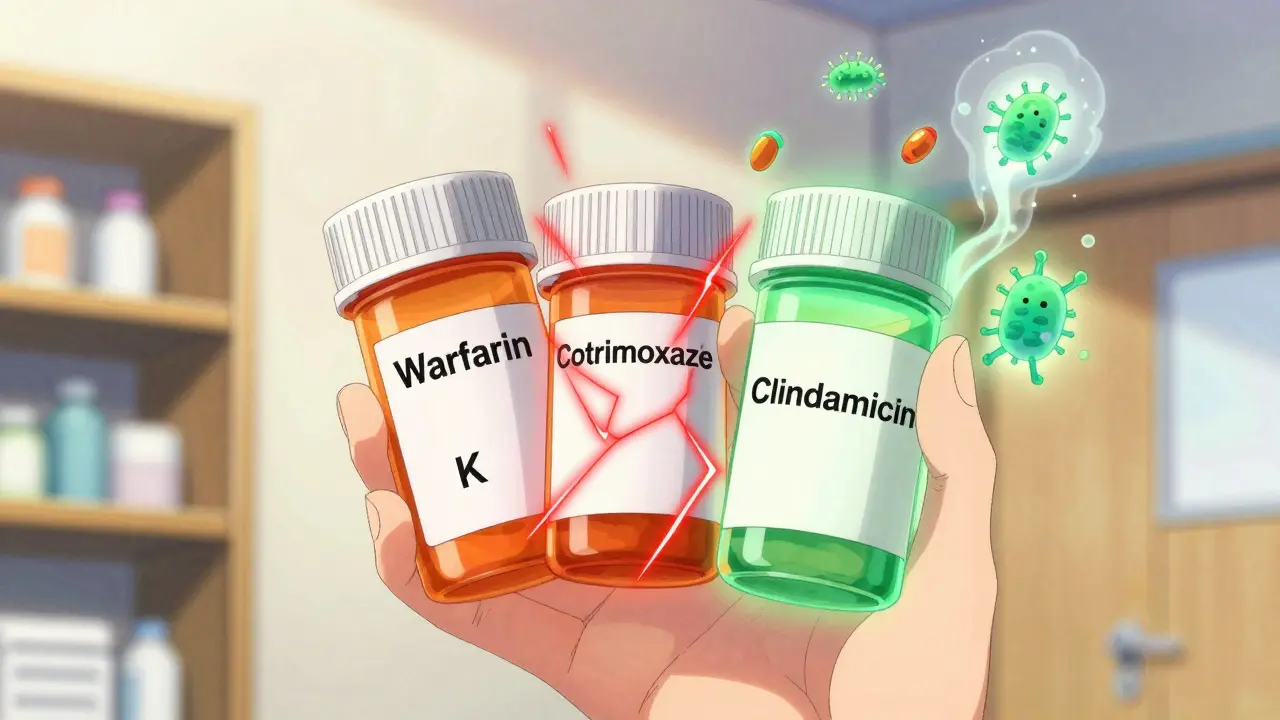
But that’s not the only mechanism. Many antibiotics also interfere with how your liver breaks down warfarin. Warfarin is processed by an enzyme called CYP2C9. Some antibiotics, like cotrimoxazole (Bactrim), ciprofloxacin, and erythromycin, block this enzyme. When that happens, warfarin sticks around longer in your body. More warfarin in your system = higher risk of bleeding.
And then there’s protein binding. Some antibiotics, especially cotrimoxazole, compete with warfarin for the same protein carriers in your blood. This temporarily increases the amount of free, active warfarin circulating - like turning up the volume on a drug you didn’t even change the dose of.
Not All Antibiotics Are Created Equal
Some antibiotics are low-risk. Others? They’re red flags.
High-risk antibiotics - these can push your INR up by more than 1.5 points in just a few days:
- Cotrimoxazole (Bactrim, Septra) - the biggest offender. Studies show it triples your risk of hospitalization for bleeding. Many clinicians reduce warfarin doses by 50% when starting this drug.
- Fluconazole - a common antifungal, but it’s a potent CYP2C9 inhibitor. Even a single dose can cause dangerous INR spikes.
Moderate-risk antibiotics - these often raise INR by 0.5 to 1.5 points:
- Fluoroquinolones (ciprofloxacin, levofloxacin)
- Macrolides (erythromycin, clarithromycin)
- Penicillins (amoxicillin, ampicillin)
- Cephalosporins (ceftriaxone, cephalexin) - these don’t affect liver enzymes much, but they wipe out gut bacteria hard.
Low-risk antibiotics - these rarely cause issues:
- Clindamycin - often the go-to for dental procedures in people on warfarin.
- Azithromycin - minimal effect on CYP2C9, so it’s safer than erythromycin.
- Metronidazole - moderate risk, but less than Bactrim. Still, monitor INR if used.
And then there’s the outlier: rifampin. This antibiotic doesn’t raise INR - it crashes it. Rifampin speeds up how fast your liver breaks down warfarin. So if you’re on rifampin for tuberculosis or a stubborn infection, your warfarin dose might need to go up - sometimes by 50% or more. And it takes weeks for your body to adjust.
What Your INR Should Do - And When to Worry
For most people, the target INR range is 2.0 to 3.0. If you’re on a mechanical heart valve, it might be 2.5 to 3.5. A single INR of 4.0 isn’t an emergency - but it’s a warning sign. An INR over 5.0 means you’re at serious risk of bleeding, even without trauma.
Here’s what to expect after starting an antibiotic:
- Days 1-2: Usually no change. Your body hasn’t had time to react.
- Days 3-5: This is when INR spikes happen. Gut bacteria die off. Liver enzymes slow down. This is the critical window.
- Days 6-10: INR may stabilize - or keep climbing if the antibiotic is still active.
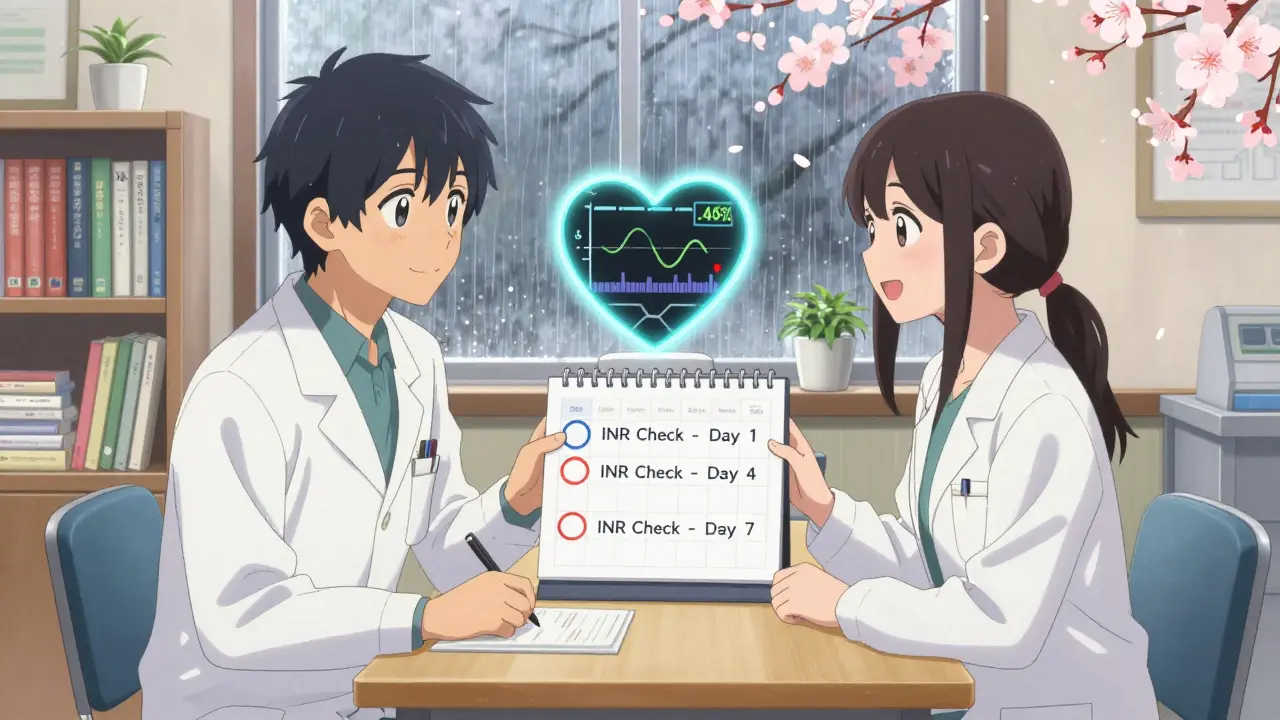
That’s why experts say: check your INR within 3 to 5 days after starting any antibiotic. Don’t wait for symptoms. Bleeding doesn’t always come with bruising or nosebleeds. Internal bleeding - in your gut, brain, or muscles - can happen silently.
What to Do When You Need Antibiotics
Don’t panic. Don’t stop warfarin. But do this:
- Know your antibiotic. Ask your doctor: “Is this one of the high-risk ones?” If they say “it’s just an antibiotic,” push back. Name the class. Ask if it affects CYP2C9 or gut flora.
- Get your INR checked before you start. This gives you a baseline. Without it, you won’t know how much the antibiotic changed things.
- Check again in 3-5 days. This is non-negotiable for moderate- and high-risk antibiotics. Many clinics now have protocols to call patients in automatically.
- Don’t adjust your dose yourself. Even if your INR is high, don’t skip a dose unless your provider tells you to. Too much reduction can lead to clots.
- Watch for signs of bleeding. Unexplained bruising, blood in urine or stool, severe headaches, dizziness, or unusual fatigue. Call your doctor immediately if you notice these.
For dental work, clindamycin is often preferred over amoxicillin for people on warfarin. Studies show it’s just as effective for preventing infection - with far less risk of INR spikes.
The Big Misconception: “I Feel Fine, So My INR Must Be Okay”
This is dangerous thinking. In a 2014 study of nearly 39,000 people on warfarin, researchers found that even when patients took high-risk antibiotics, most didn’t have symptoms before their INR went up. No bleeding. No bruising. Just a lab result that told a different story.
That’s why monitoring beats symptoms every time. You can feel perfectly fine and still be at risk. Your body doesn’t always warn you before something serious happens.
What About DOACs? Are They Safer?
Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran have become popular because they don’t need regular INR checks. But they’re not magic. Some DOACs still interact with antibiotics - especially those that affect liver enzymes or kidney function. For example, rifampin can make rivaroxaban less effective. And some antibiotics can increase bleeding risk with DOACs too.
If you’re on a DOAC, you’re not off the hook. You still need to tell your doctor you’re on blood thinners before starting any antibiotic. The rules are just different.
Bottom Line: Stay Alert, Don’t Panic
Warfarin and antibiotics can coexist safely - if you’re smart about it. The key isn’t avoiding antibiotics. It’s knowing which ones are risky, checking your INR at the right time, and working with your care team to adjust doses when needed.
Most people who take antibiotics while on warfarin never have a problem. But those who do? They often didn’t get their INR checked. That’s the gap. Not the medication. Not the infection. The missed test.
So next time your doctor prescribes an antibiotic, ask: “Could this affect my warfarin?” Then ask: “When should I get my INR checked?” That simple conversation could prevent a hospital visit - or worse.
What If You’re on Warfarin and Need Surgery?
If you’re scheduled for surgery - even a simple dental extraction - your care team should check your INR 24-48 hours before the procedure. Many surgeons prefer an INR under 1.5 for minor procedures. But stopping warfarin too early increases clot risk. The best approach? Keep taking warfarin, monitor INR closely, and use local measures like sutures or tranexamic acid mouthwash to control bleeding. Don’t stop your medication without clear direction from your anticoagulation provider.
Can I take over-the-counter painkillers while on warfarin and antibiotics?
Avoid NSAIDs like ibuprofen or naproxen. They increase bleeding risk on their own and can make warfarin effects worse. Acetaminophen (paracetamol) is safer, but don’t exceed 3,000 mg per day - high doses can also affect liver enzymes and INR. Always check with your pharmacist before taking any OTC medicine.
How long after stopping an antibiotic does my INR go back to normal?
It depends on the antibiotic. For most, INR starts dropping within 3-7 days after stopping. But if you took a drug like rifampin that made your body break down warfarin faster, it can take 2-4 weeks for your liver enzymes to return to normal. Always recheck your INR after finishing the antibiotic - don’t assume it’s back to baseline.
Is it safe to take probiotics while on warfarin and antibiotics?
Probiotics may help restore gut bacteria after antibiotics, but there’s no strong evidence they prevent INR spikes. Some strains produce vitamin K, so theoretically they could reduce warfarin’s effect - but this is unpredictable. Don’t rely on them to fix your INR. Stick to monitoring and medical advice.
What should I do if my INR is too high but I’m not bleeding?
If your INR is between 4.0 and 5.0 and you have no bleeding, your provider may advise skipping one or two warfarin doses and rechecking in 2-3 days. For INR above 5.0, they might give vitamin K orally. Never take vitamin K on your own - too much can make warfarin ineffective and cause clots. Always follow your care team’s instructions.
Can I drink alcohol while on warfarin and antibiotics?
Moderate alcohol (one drink per day) is usually okay, but heavy drinking can raise INR by affecting liver function and reducing vitamin K absorption. Alcohol also increases bleeding risk on its own. Avoid binge drinking, especially when you’re on antibiotics - your liver is already under stress.
Final Thought: It’s Not About Avoiding Antibiotics - It’s About Managing Risk
Antibiotics save lives. Warfarin saves lives. The problem isn’t the drugs. It’s the lack of awareness. You don’t need to avoid antibiotics if you’re on warfarin. You need to know which ones are risky, when to test your INR, and how to respond.
That’s the real takeaway. It’s not magic. It’s not complicated. It’s simple: test early, monitor often, communicate clearly. Do that, and you’ll stay safe - even when you need to take both.


Did you know the FDA quietly changed the warfarin guidelines in 2021 but never told the public? I found a leaked memo from a pharma exec saying they pushed DOACs because they make more money off monthly prescriptions than once-a-week INR checks. They don’t want you monitoring your own blood-they want you dependent on labs and doctors who bill for every test. I’ve been on warfarin for 12 years and I check my INR at home with a portable device. No one in my doctor’s office even knows I do it. They think I’m just lucky. I’m not. I’m awake.
There is a fundamental error in your assertion that 'cotrimoxazole triples the risk of hospitalization for bleeding.' The actual study you reference (Lancet 2017) reports a hazard ratio of 2.98-not 'tripled'-and this was adjusted for age, renal function, and concomitant NSAID use. Furthermore, the term 'high-risk antibiotics' is misleading; risk is context-dependent. A 72-year-old with CHF and CKD on Bactrim is at high risk. A 34-year-old with no comorbidities is not. Precision matters. Sloppy language erodes trust in medical communication.
The human body is not a machine with discrete inputs and outputs. Warfarin, antibiotics, gut flora, liver enzymes-they exist in a dynamic equilibrium shaped by diet, sleep, stress, and even the seasons. To reduce this to a list of 'high-risk' and 'low-risk' drugs is to misunderstand the nature of biological systems. The real danger lies not in the antibiotics, but in the reductionist mindset that believes we can control complex physiology with checklists. Perhaps we should ask not 'which antibiotic is safest?' but 'how can we restore balance rather than override it?'
Everyone says 'check your INR' like it's that easy. What if you live in a rural area and the nearest lab is 90 minutes away? What if you're on Medicaid and they won't cover it unless you're actively bleeding? And don't get me started on how doctors act like you're being dramatic when you ask for a test before starting an antibiotic. It's not paranoia. It's survival. The system is rigged to ignore people like us until it's too late.
Okay but have you considered that maybe we’re all just supposed to be on DOACs now and this whole warfarin thing is just a relic from the 90s? Like why are we still doing this? 🤔
lol so many ppl think antibiotics are just pills u take but they dont know the gut is a whole other body. i read on a forum that bactrim kills ur good bacteria so bad u get yeast infections and then u start takin antifungals and then ur inr goes nuts again. its like a domino effect. and no one talks about it. just me? 🤷♂️
Let’s be real-most people on warfarin don’t even know what INR stands for. I’ve seen patients bring in their own INR logs and they’ve written ‘normal’ or ‘good’ instead of numbers. And then they’re mad when they bleed. You can’t outsource your health to a doctor who spends 7 minutes with you. This isn’t about antibiotics. It’s about people refusing to take responsibility for their own bodies. You want to live? Learn. Or don’t. But don’t act surprised when things go wrong.
I’ve been on warfarin since my mechanical valve replacement in 2018. The first time I got antibiotics for a sinus infection, my INR jumped to 6.2. I didn’t feel a thing. No bruising, no nosebleeds, nothing. That scared me more than anything. Since then, I’ve built a little spreadsheet: antibiotic, date started, date of next INR, and what my doctor told me to watch for. It’s not glamorous, but it’s kept me alive. If you’re on warfarin, do the spreadsheet. It’s the bare minimum.
Wow. So the American medical system has created an entire industry around monitoring blood thinners, while in the UK we just prescribe DOACs and move on. You people turn a simple medical decision into a 10-page PDF with flowcharts. I mean, really. We don’t need a PhD to know that if you’re on blood thinners, you don’t take Bactrim. It’s not rocket science. Just stop overcomplicating things.
You’re not alone. I had a friend who almost bled out after taking amoxicillin and didn’t get her INR checked. She’s fine now, but it took three units of blood and a night in the ICU. Please, if you’re reading this-don’t wait for symptoms. Test early. Test often. Your life is worth more than your convenience.
There is value in both sides. The structured approach of INR monitoring saves lives. But so does the intuitive understanding that our bodies are not machines. Perhaps the future lies in combining precision medicine with holistic awareness-not just which antibiotic, but how you’re sleeping, how much vitamin K you ate, whether you’re stressed. Medicine needs both the algorithm and the human touch.
DOACs are not safer. They are more expensive. They are not reversible. They are not monitored. You think you are avoiding INR checks but you are trading one risk for a silent, unmeasurable one. The system pushes DOACs because they are profitable. Not because they are better. Question everything. Especially the things they tell you are simple.