Antidepressant & Birth Control Interaction Checker
Check Your Medication Combination
Select your antidepressant type and birth control method to see if there's a risk of interactions.
Many women take both antidepressants and birth control at the same time. It’s not unusual. About 10.4% of women between 18 and 39 in the U.S. are on antidepressants, and nearly 90% of women use some form of birth control during their reproductive years. When these two medications overlap, questions naturally come up: Does one make the other less effective? Do side effects get worse? Is it safe to take them together?
Most Antidepressants Don’t Break Birth Control
The good news? For most women, taking common antidepressants like SSRIs (Selective Serotonin Reuptake Inhibitors) - such as sertraline (Zoloft), fluoxetine (Prozac), or escitalopram (Lexapro) - doesn’t reduce the effectiveness of hormonal birth control.A 2024 review of 15 clinical studies involving over 3,800 women found no statistically significant drop in contraceptive effectiveness when SSRIs were taken with combined oral contraceptives. In one study, women taking fluoxetine alongside birth control had an unintended pregnancy rate of 0.9%, compared to 0% in the placebo group - a difference too small to be meaningful.
Doctors often see this combination in practice. Women with anxiety, depression, or PMDD (premenstrual dysphoric disorder) benefit from SSRIs, and many also want reliable birth control. The FDA’s prescribing information for Lexapro even states: “No dose adjustment is necessary when co-administered with oral contraceptives.” That’s not a minor note - it’s a clear signal from regulators that this pairing is considered safe.
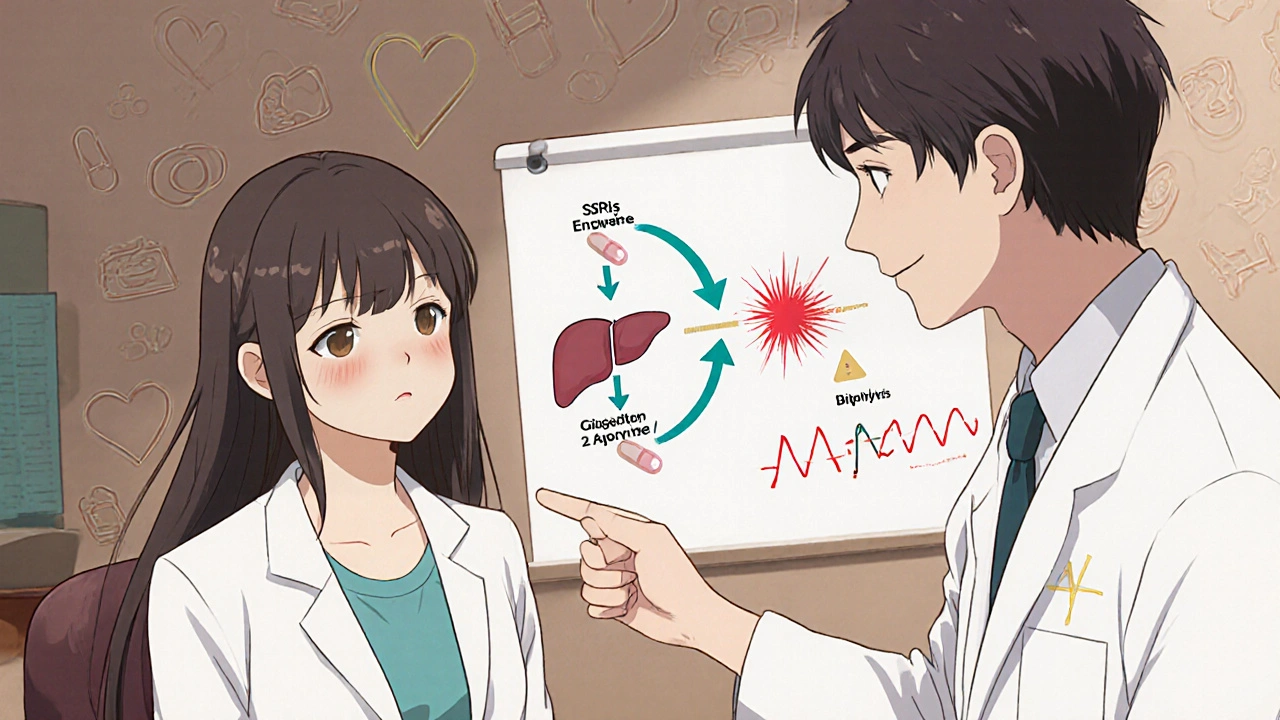
Where the Real Risk Lies: Tricyclic Antidepressants
Not all antidepressants are the same. Tricyclic antidepressants (TCAs) (like amitriptyline, nortriptyline, and imipramine) are a different story. These older medications are metabolized by liver enzymes - specifically CYP1A2 and CYP2C19 - that are also affected by estrogen in birth control pills.When estrogen blocks these enzymes, TCAs can build up in the bloodstream. Studies show this can increase TCA levels by 30% to 50%. That might not sound like much, but for drugs with a narrow safety margin, even small changes matter. Higher levels raise the risk of side effects like dizziness, dry mouth, blurred vision - and more seriously, QT prolongation, a heart rhythm issue that can lead to dangerous arrhythmias.
A 2019 study found that 12% of patients on TCAs and birth control showed signs of QT prolongation on EKGs. That’s why many doctors avoid prescribing TCAs to women on hormonal contraception. If you’re on amitriptyline and your doctor suggests switching to sertraline, it’s not just a random change - it’s a safety move.
What About Bupropion?
Bupropion (Wellbutrin) is an atypical antidepressant that doesn’t work like SSRIs. It doesn’t boost serotonin - it targets dopamine and norepinephrine. That also means it doesn’t interfere with the same liver enzymes as SSRIs or TCAs.Studies show bupropion causes less than 5% variation in estrogen levels when taken with birth control. That’s negligible. It’s also one of the few antidepressants that doesn’t commonly cause sexual side effects like low libido or trouble reaching orgasm - a major plus for women who already experience reduced desire from hormonal birth control.
If you’re struggling with sexual side effects from SSRIs and birth control together, switching to bupropion is one of the most effective solutions. A 2022 survey found that 41% of women on both medications reported compounded sexual dysfunction. Bupropion’s sexual side effect rate is only around 20% - nearly half that of SSRIs.
Birth Control Type Matters Too
Not all birth control is made the same. Combined hormonal methods - pills, patches, rings - contain estrogen and progestin. Progestin-only methods - the mini-pill, implants like Nexplanon, or the hormonal IUD (Mirena, Kyleena) - don’t have estrogen.Estrogen is the part that can interfere with how the liver processes certain drugs. That’s why progestin-only methods have even fewer documented interactions. A 2023 clinical review from Nurx found no significant changes in hormone levels or contraceptive effectiveness when SSRIs were taken with implants or hormonal IUDs.
Women who’ve had bad reactions to estrogen - like migraines with aura, blood clots, or high blood pressure - often switch to progestin-only options anyway. For them, combining these with SSRIs is not just safe - it’s often the best choice.
What About Other Medications?
You might be taking more than just antidepressants and birth control. Some antibiotics, like rifampin (used for tuberculosis), can drastically reduce birth control effectiveness by speeding up how fast your body breaks down estrogen. Studies show a 60% drop in estrogen levels with rifampin.But common antibiotics like amoxicillin, azithromycin, or ciprofloxacin? No effect. You don’t need backup birth control if you’re on these.
Antipsychotics like risperidone can increase prolactin levels - a hormone that affects menstruation and milk production. When combined with birth control, this effect might be stronger, but the evidence is mostly from case reports, not large studies. Still, if you’re on an antipsychotic and notice missed periods or breast changes, talk to your doctor.
Overlapping Side Effects Are Common - and Manageable
The biggest issue isn’t usually effectiveness. It’s side effects.SSRIs can cause nausea, weight gain, fatigue, and sexual dysfunction. Birth control can cause mood swings, bloating, headaches, and reduced libido. When you take both, these can pile up.
A 2022 Healthline survey of 1,243 women found:
- 68% saw no change in birth control effectiveness
- 22% had more breakthrough bleeding
- 10% felt worse mood swings
- 37% reported decreased libido
That last one is key. Sexual side effects from SSRIs affect 30-70% of users. Hormonal birth control reduces sexual desire in 15-25%. Together? It’s no surprise that nearly half of women feel this double hit.
Here’s what helps:
- Switch from an SSRI to bupropion
- Switch from a pill to a non-hormonal IUD (like the copper IUD)
- Try a lower-dose birth control option
- Give it time - side effects often fade after 6-8 weeks
What Your Doctor Should Do
Good care means more than just writing a prescription. Your provider should:- Ask if you’re on birth control before starting an antidepressant
- Check your liver function if you’re on a TCA
- Monitor mood and menstrual patterns in the first 2-3 months
- Warn you about overlapping side effects, especially sexual ones
- Offer alternatives if things aren’t working
Many doctors don’t bring this up unless you do. Don’t be shy. Say: “I’m on birth control. Will this antidepressant affect it?” That’s a smart, normal question.
What You Can Do Right Now
If you’re taking both medications:- Keep track of your mood, bleeding patterns, and sexual desire. Note any changes in a journal or app.
- Don’t stop either medication suddenly. That can cause withdrawal or rebound depression.
- Take your pills at the same time every day. Some experts suggest spacing them 2 hours apart to avoid stomach upset, but there’s no proof it helps with interactions.
- Call your doctor if you have new or worsening side effects - especially chest pain, irregular heartbeat, severe mood changes, or heavy bleeding.
- Ask about your options: Is there a different antidepressant? A non-hormonal birth control method?
Remember: You’re not alone. Millions of women manage both mental health and birth control at the same time. The goal isn’t perfection - it’s finding a balance that works for you.
Frequently Asked Questions
Can antidepressants make birth control less effective?
For most common antidepressants - especially SSRIs like sertraline, fluoxetine, and escitalopram - no. Research shows no meaningful drop in contraceptive effectiveness. The exception is tricyclic antidepressants (TCAs) like amitriptyline, which can build up in your system when combined with estrogen-containing birth control, potentially increasing side effects but not reducing pregnancy prevention.
Does Lexapro interfere with birth control?
No. Lexapro (escitalopram) does not interfere with the effectiveness of birth control pills, patches, rings, or IUDs. The FDA’s prescribing information confirms no dose adjustment is needed. Studies show no significant change in hormone levels or pregnancy rates when taken together.
Can birth control make depression worse?
For some women, yes. Hormonal birth control can trigger or worsen mood symptoms, especially in those with a history of depression or PMDD. If you notice increased sadness, irritability, or anxiety after starting birth control, talk to your doctor. Switching to a lower-dose pill or a non-hormonal method like the copper IUD may help.
Do SSRIs cause sexual side effects with birth control?
Yes - and it’s common. SSRIs are known to reduce libido and cause difficulty with arousal or orgasm. Birth control can also lower sexual desire in some women. When combined, these effects can multiply. About 41% of women report compounded sexual side effects. Switching to bupropion (Wellbutrin) or switching to a non-hormonal birth control method can help reduce this overlap.
Should I take my antidepressant and birth control at the same time?
You can, but spacing them out by 2 hours may help reduce stomach upset - though it won’t prevent drug interactions. The real concern isn’t timing - it’s which medications you’re taking. If you’re on a TCA like amitriptyline, talk to your doctor about switching to a safer option like sertraline or bupropion.
What’s Next?
Research is still evolving. New antidepressants like vortioxetine and levomilnacipran haven’t been studied as much in combination with birth control. Genetic testing for liver enzyme variations (like CYP2D6 and CYP2C19) may one day help predict who’s at risk for interactions - but it’s not routine yet.For now, the message is clear: You don’t have to choose between mental health and reproductive control. With the right medication choices and open communication with your provider, you can manage both safely and effectively.


From a pharmacokinetic standpoint, the CYP450 enzyme system is the linchpin here. SSRIs like sertraline are weak inhibitors of CYP2D6 and CYP3A4, but they don't significantly alter the metabolism of ethinyl estradiol or norethindrone. The 2024 meta-analysis you cited is robust-no clinically relevant pharmacodynamic interference. The real clinical concern is pharmacodynamic overlap: serotonin modulation + hormonal flux = potential for emotional lability. That’s why bupropion’s dopaminergic profile is so advantageous-it avoids the serotonergic cascade entirely while preserving contraceptive efficacy. Progestin-only methods further mitigate risk by eliminating estrogen-mediated CYP1A2 suppression. This isn’t just safe-it’s elegant pharmacotherapy.
It’s strange how we treat the body like a machine with interchangeable parts. We stack drugs like Lego blocks and expect harmony. But depression isn’t just a chemical imbalance-it’s a lived experience. Birth control isn’t just contraception-it’s control over time, over identity. When we say ‘no interaction,’ are we really saying ‘no consequence’? Maybe the real interaction is between societal expectations and our willingness to medicate everything. We don’t ask enough what these pills are doing to our souls, not just our livers.
SSRIs are just chemical crutches. People should just go to therapy and stop being so weak.
Let me be clear: the FDA doesn't have your best interests at heart. They approved Lexapro with birth control because Big Pharma owns them. The real data is buried. You think 0.9% pregnancy rate is safe? That's 1 in 111 women getting pregnant because they were misled. And don't get me started on the 12% QT prolongation stat-those numbers are being buried under glossy brochures. Wake up. This isn't medicine. It's corporate manipulation dressed in white coats.
As an American who actually understands science, I find it embarrassing that people still question this. The data is overwhelming. The U.S. has the most rigorous drug approval system in the world. If the FDA says no dose adjustment is needed, that’s the end of the conversation. Anyone who doubts this is either misinformed or ideologically opposed to modern medicine. We don’t need anecdotal horror stories from Reddit-we need evidence. And the evidence says: safe. Period.
Okay but like… did anyone notice that the article says ‘10.4% of women 18-39 are on antidepressants’ but then says ‘90% use birth control’? That means like… 9% of women are on BOTH? That’s like 8 million women? But then they say ‘no interaction’? But I read on a blog that Lexapro makes your boobs leak? And my cousin’s friend’s dentist said SSRIs cause autism in babies? Also why is everyone so obsessed with sex? Can’t we just be happy? I’m not even sure I believe any of this anymore. Also I think the moon is fake.
Bro this is why Africa can’t progress. You people take so many pills you forget how to feel natural. In Nigeria, we fix depression with prayer, yam, and walking barefoot. Birth control? We use tradition. Why you always need chemical fix? You think your liver is a factory? 😅
Interesting how the article focuses on SSRIs and TCAs but omits SNRIs. Venlafaxine, for instance, has a more complex interaction profile due to its dual inhibition of serotonin and norepinephrine reuptake, and its metabolite, desvenlafaxine, is metabolized by CYP2D6-same pathway affected by estrogen. There’s limited data, but a 2021 case series noted elevated venlafaxine concentrations in patients on combined oral contraceptives, with mild serotonin-related side effects. Not as pronounced as TCAs, but worth monitoring. Also, progestin-only IUDs are ideal for patients on polypharmacy due to minimal hepatic involvement.
I just want to say-this article saved me. I was terrified to keep taking my antidepressant because I heard it would mess with my IUD. Turns out, it’s fine. I’ve been on sertraline and Kyleena for two years. My mood is stable, no breakthrough bleeding, and I finally feel like myself again. If you’re reading this and scared-talk to your doctor. You don’t have to choose between being mentally well and being in control of your body. You deserve both.
Why are we even talking about this like its a mystery? Everyone knows SSRIs kill your sex drive and birth control makes you moody so you just end up numb. Thats the real side effect. Nobody wants to admit it but its just a chemical zombie state. Just take a break. Go outside. Eat real food. Stop taking everything. The system wants you dependent
As a clinical pharmacologist with 17 years in academic research, I must emphasize that the data on SSRIs and hormonal contraception is not only robust but also clinically reassuring. The pharmacokinetic profiles of escitalopram, sertraline, and fluoxetine demonstrate negligible CYP3A4 induction or inhibition, and estrogen’s effect on hepatic metabolism is functionally insignificant at therapeutic doses. Furthermore, the 2022 Healthline survey’s 37% libido reduction statistic is misleading-it conflates baseline hormonal suppression with pharmacological interaction. The real issue is psychosocial: women internalize sexual dysfunction as personal failure rather than recognizing it as a common, reversible side effect. Switching to bupropion or a copper IUD is not a compromise-it’s a strategic recalibration of therapeutic goals. And yes, spacing doses by two hours is a myth. Take them together. Your liver isn’t that fragile.
I’ve been on Lexapro and the Mirena for three years. Zero issues. No mood swings, no bleeding, no weird side effects. I wish more people knew this was normal. You can take care of your mental health AND your body. No shame in that.