Every year, hundreds of thousands of people in the U.S. are harmed by mistakes in their prescriptions-not because the medicine is dangerous, but because the prescription itself was written wrong. These aren’t rare glitches. They’re common, preventable, and often hidden in plain sight. You might not know it, but you hold more power than you think to stop these errors before they reach your medicine cabinet.
What Exactly Goes Wrong in a Prescription?
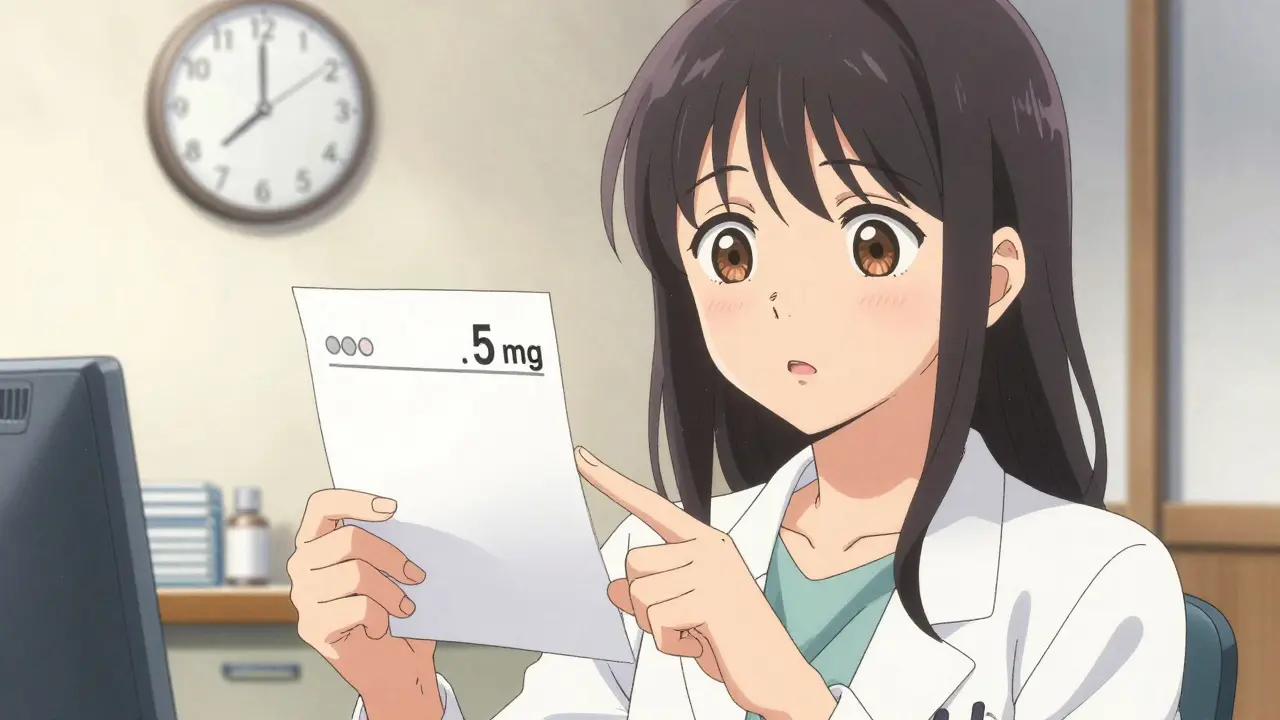
Prescription errors happen before the pharmacist even sees the paper or digital order. They come from the doctor’s office, clinic, or hospital, and they’re not always about bad intentions. Most are slips caused by time pressure, messy handwriting, or confusing shortcuts.One of the most dangerous mistakes? Writing ‘U’ for units. That tiny letter can be mistaken for a zero, turning a 5-unit insulin dose into 50 units-enough to send someone into a life-threatening coma. Or writing ‘.5 mg’ without a zero in front. That gets read as ‘5 mg’-ten times too strong. The FDA says these decimal errors caused 128 deaths between 2010 and 2020.
Then there’s drug name confusion. Celebrex and Celexa look and sound alike. Zyprexa and Zyrtec? Same thing. One treats arthritis. The other treats allergies. Mix them up, and you’re giving a heart patient an antihistamine that could raise their blood pressure dangerously. A 2022 study found these look-alike/sound-alike mix-ups make up 25% of all prescribing errors.
And don’t forget the abbreviations. ‘QD’ means once daily-but if it’s misread as ‘QID’ (four times daily), you’re doubling or tripling your dose. ‘MS’ could mean morphine sulfate or magnesium sulfate. One calms pain. The other stops seizures. Confusing them? That’s a medical emergency.
Who’s Responsible? And Why Does This Keep Happening?
It’s easy to blame the doctor. But the system is stacked against them. A 2021 study found physicians in busy clinics spend just 17 seconds per prescription. That’s less time than it takes to microwave a cup of coffee. With 20+ patients a day, 10+ medications to check for interactions, and electronic systems full of dropdown menus that look almost identical, mistakes are almost guaranteed.Even when doctors use electronic prescribing, new problems pop up. A 2019 study in JAMA Internal Medicine found that while e-prescribing cut handwriting errors by 55%, it created 34% new types of mistakes. Why? Dropdown menus. You’re looking for ‘Lisinopril 10 mg’-but the list shows ‘Lisinopril 5 mg’ right above ‘Lisinopril 20 mg.’ Your finger slips. You pick 20 mg. Boom. Double dose. And 31% of providers just turn off safety alerts because they get too many false alarms.
High-alert drugs are the worst offenders. Insulin, blood thinners like warfarin, and opioids like oxycodone make up only 8% of all prescriptions-but 72% of fatal errors. That’s because even a small mistake can kill.
What Should You Look For on Your Prescription?
You don’t need to be a doctor to spot red flags. Here’s a simple checklist you can use every time you get a new prescription:- Full drug name-not an abbreviation. ‘Metformin,’ not ‘Glucophage’ (which is the brand name). Avoid anything that looks like ‘Lasix’-it should say ‘Furosemide.’
- Precise dosage-Always written with a leading zero for decimals under 1. ‘0.5 mg’ not ‘.5 mg.’ No trailing zeros. ‘5 mg’ not ‘5.0 mg.’
- Clear frequency-No ‘QD,’ ‘BID,’ or ‘TID.’ It should say ‘once daily,’ ‘twice daily,’ or ‘three times daily.’
- Total quantity-If you’re on a 30-day course, does the script say 30 pills? If it says 90, ask why.
- Reason for the medicine-It should say something like ‘for high blood pressure’ or ‘for type 2 diabetes.’ If it’s blank, ask.
- Prescriber’s info-Name, phone number, license number. If it’s missing, the script might be fake or altered.
- Expiration date-Prescriptions expire. Most are good for 6-12 months. If it’s old, ask if you still need it.
Use this checklist before you even leave the doctor’s office. If you’re handed a handwritten script, ask if they can print it out or send it electronically. Handwritten prescriptions still cause 22% of all errors.

How to Verify Your Prescription at the Pharmacy
The pharmacy isn’t the final checkpoint-it’s your last chance to catch an error before you take the medicine. Don’t just grab the bottle and walk out.When the pharmacist hands you the bottle, compare the label to your checklist. Does the name match? The dose? The number of pills? If it’s insulin, is it clearly labeled as ‘insulin’ and not ‘heparin’? If it’s a blood thinner, is the dose exactly what your doctor told you?
Use the teach-back method. Say out loud: ‘So this is metformin 500 mg, two pills twice a day with meals, for my diabetes, right?’ If the pharmacist nods and says yes, you’re good. If they hesitate, ask again. A Johns Hopkins study showed this simple trick cuts misunderstandings by 81%.
For electronic prescriptions, check your pharmacy’s app or portal. Many now show you the original e-prescription sent by your doctor. Compare it to what you received. If the dose is different, call your doctor’s office immediately.
High-Risk Drugs: Know the Dangerous Pairs
Some medications are more dangerous when mixed up. The Institute for Safe Medication Practices keeps a public list of these ‘error-prone pairs.’ Here are a few you should know:- Lamotrigine (for seizures) vs. Lamictal (the brand name)-if the script says Lamictal without the dose, you might get 200 mg instead of 25 mg. That’s a 10-fold overdose risk.
- Hydrocortisone (skin cream) vs. Heparin (blood thinner)-both can be written as ‘HC.’ One treats rashes. The other prevents clots. Mix them up and you could bleed internally.
- Insulin (for diabetes) vs. heparin (for clots)-both are injectable. Both come in similar vials. One can kill you if given by mistake.
When you get a new prescription for any high-alert drug, ask: ‘Is this one of the drugs that’s commonly mixed up with another?’ Most pharmacists will know the list. If they don’t, ask for the ISMP’s error-prone drug pairs guide. It’s free online.

What to Do If You Spot an Error
Don’t assume it’s your fault. Don’t take the medicine if something feels off. Don’t wait until the next appointment.Call your doctor’s office right away. Say: ‘I received a prescription for [drug name], but the dose says [wrong dose]. I think it might be wrong. Can you please confirm?’ Most offices have a nurse or pharmacist on call who can fix it within an hour.
If you’re at the pharmacy and the label doesn’t match what your doctor told you, don’t take it. Ask the pharmacist to call the prescriber. Pharmacies are required to verify prescriptions before dispensing. If they refuse, ask to speak to the pharmacy manager.
And if you’re ever unsure-ask again. Always. There’s no such thing as a dumb question when your life is on the line.
Tools That Can Help You
You don’t have to do this alone. There are tools now designed to help patients catch errors:- MedSafety app-Scan your prescription with your phone camera. The app uses AI to detect common errors like missing zeros, wrong units, or confusing abbreviations. In a 2023 pilot, it caught 68% of errors patients missed.
- Text alerts from your provider-Some clinics now send automated SMS messages after a prescription is sent. It says: ‘Your new prescription: Metformin 500 mg, two pills daily, for diabetes. Expires 6/30/2026.’ If the text doesn’t match what you got, you know to call.
- ‘Ask Me 3’ program-Before you leave the doctor’s office, ask: ‘What is my main problem?’ ‘What do I need to do?’ ‘Why is it important?’ A 2021 study showed patients who asked these three questions reduced their medication errors by 44%.
These tools aren’t magic. But they turn you from a passive receiver into an active partner in your care.
Why This Matters More Than You Think
Medication errors cost the U.S. healthcare system $42 billion a year. That’s more than the entire annual budget of Australia’s public health system. But behind every dollar is a person-someone who had a stroke because they got the wrong blood thinner, someone who went into a coma because they took ten times their insulin dose, someone who died because a doctor wrote ‘U’ instead of ‘units.’And here’s the truth: 50% of these errors can be prevented if patients speak up. That’s not a guess. It’s from the Agency for Healthcare Research and Quality. You don’t need to be a doctor. You don’t need to know Latin terms or pharmacology. You just need to look, listen, and ask.
By 2027, patient verification will be standard. Hospitals and insurers are already building systems that require your digital confirmation before a prescription is filled. But you don’t have to wait. Start today. Check your next script. Ask the questions. Save your life-or someone else’s.
What are the most common prescription writing errors?
The most common errors include wrong dosage (especially with decimals like .5 mg read as 5 mg), confusing drug names (like Celebrex vs. Celexa), dangerous abbreviations (like ‘U’ for units or ‘QD’ for daily), and missing information like the reason for the drug. Handwriting issues and electronic system dropdown mistakes are also top culprits.
Can I trust my pharmacist to catch prescription errors?
Pharmacists are trained to catch errors, and they do-about 41% of prescription errors are caught at the pharmacy. But they’re overwhelmed. Pharmacies now spend nearly 19 minutes per prescription on verification, up from 6 minutes in 2015. You shouldn’t rely on them alone. Always double-check yourself using the seven-point checklist.
What should I do if my prescription looks wrong?
Don’t take it. Call your doctor’s office immediately. Say exactly what you see: ‘The script says 50 mg, but I was told 5 mg.’ Ask them to confirm or correct it. If you’re at the pharmacy, ask them to call the prescriber before filling it. You have the right to refuse a medication if it doesn’t match what you expect.
Are electronic prescriptions safer than handwritten ones?
Yes and no. Electronic prescriptions cut handwriting errors by 55%, but they introduced new problems like dropdown menu mistakes and alert fatigue. Providers often bypass safety alerts, leading to 15,000 preventable errors every month. Always compare the printed label to the e-prescription details in your patient portal.
How can I tell if a drug is high-risk?
High-risk drugs include insulin, blood thinners (warfarin, apixaban), opioids (oxycodone, fentanyl), and seizure medications (lamotrigine). These are listed by the Institute for Safe Medication Practices. If you’re prescribed one, ask: ‘Is this one of the drugs that’s commonly confused with another?’ Always verify the dose and purpose.
What’s the ‘teach-back method’ and how do I use it?
The teach-back method means you repeat back what you were told in your own words. After your doctor or pharmacist explains your prescription, say: ‘So this is [drug name], [dose], [frequency], for [reason], right?’ If they say yes, you’re clear. If they correct you, you’ve caught an error. This reduces misunderstandings by 81%.

This is exactly why I refuse to take anything without checking the label three times. I had a nurse hand me a vial labeled 'Heparin' and I asked if it was insulin. She froze. Turned out it was. I didn't take it. I live because I didn't trust the system.
The system is broken and everyone knows it. Doctors rushed pharmacists overwhelmed patients clueless. You want change? Stop blaming individuals. Fix the workflow. Stop the dropdowns. Stop the abbreviations. Done.
Man i just got back from the doc and i swear i thought my script said 'Lamictal' but the bottle said 'Lamotrigine' and i was like wait is this the same thing? Turns out it is but the pharmacist had to explain it like i was five. Why do we still do this? Why not just print the generic name on everything?
I used to think pharmacists were superheroes. Then I worked in a pharmacy. They're overworked, underpaid, and forced to ignore 90% of their own safety alerts because they're drowning in false alarms. It's not their fault. It's the EHR's fault. And the FDA's fault. And the insurance companies' fault. We're all just trying not to die.
The prevalence of look-alike/sound-alike medication errors remains a persistent threat to patient safety. According to the Institute for Safe Medication Practices, these errors are statistically significant and disproportionately affect high-alert medications. The implementation of standardized nomenclature and electronic prescribing with decision support is empirically supported as a mitigation strategy.
I used to think I was just paranoid... until my grandma almost died because her 'insulin' was labeled 'heparin' and the pharmacy didn't catch it. 🥲 Now I read every label like it's a bomb defusal manual. And I make my mom repeat back what the doctor says. It's not weird. It's survival. We have to be our own last line of defense.
Americans think they can outsmart systemic failure by reading labels. This is not a patient problem. This is a structural collapse of medical infrastructure. In South Africa we have no electronic systems but we have trained nurses who verify every script by hand. You don't need AI. You need people who are paid to care.
i never knew about the .5 mg thing until my friend took 5mg by mistake and ended up in er. now i always check for leading zero. also i use medsafety app and it saved me twice. thanks for this post man. really helpful. i think everyone should know this
The real issue isn't the prescription. It's the commodification of care. When your doctor has 17 seconds per patient, you're not a person. You're a data point. And when the system treats life like a spreadsheet, errors aren't mistakes. They're inevitable outcomes.
You think this is bad? Try getting a prescription in India where doctors write in Hindi and English mixed and the pharmacy staff guesses the dose. At least here you have apps and labels. We have handwritten scripts with no name and a scribble for dosage. You're lucky you're in the US
I asked for my blood pressure med. Got oxycodone. Called the doc. They laughed. Said I must’ve misheard. I didn’t. I still have the bottle.
I love how this post makes it sound like patients are the solution. Meanwhile, doctors are being pushed to write 100 scripts a day while getting yelled at by insurance companies. You’re not a hero for checking your pill bottle. You’re just surviving a broken system.
This entire article is performative safety theater. The real problem is that we treat medicine like a consumer product. You don't fix errors by teaching patients to read labels. You fix them by paying doctors to think, not click.
I read this and thought wow this is so important. Then I remembered my doctor doesn't even speak English. He just taps on his tablet and the pharmacy gets it. No one checks. No one cares. This is a luxury for people who can afford to ask questions.
I showed my mom this checklist. She’s 72. She took her meds for 20 years without ever questioning anything. Now she calls the pharmacy every time. She says 'I’m not dying because someone clicked the wrong box.' I’m proud of her.