Living with proctitis is a chronic inflammation of the rectal lining that can cause pain, bleeding, and frequent bathroom trips. It is classified under inflammatory bowel disease (IBD) and often requires medication, dietary tweaks, and lifestyle changes. When the symptoms flare up, it can feel like you’re navigating a maze alone. That’s why a reliable proctitis support network can turn isolation into empowerment.
Why a Support Network Matters
A support network does more than just listen. It supplies practical tips, emotional reassurance, and sometimes even medical guidance. Research from the American Gastroenterological Association shows that patients with strong peer connections report 30% fewer emergency visits related to IBD flare‑ups. In other words, the people you surround yourself with can directly influence your health outcomes.
Types of Support You Can Tap Into
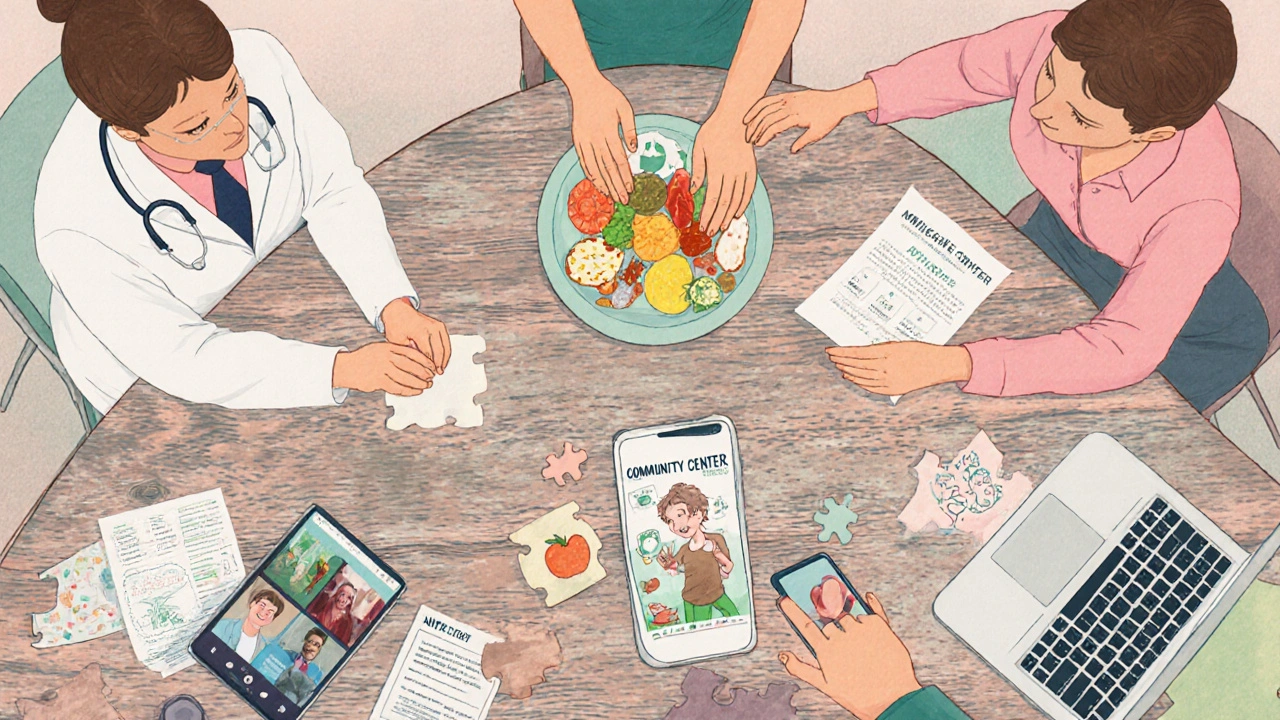
Think of support as a toolkit. Here are the main categories you’ll want to consider:
- Medical support includes specialists like a gastroenterologist who can tailor medication and monitor disease progression.
- Nutritional guidance from a nutritionist who knows which foods can soothe the gut and which can trigger flare‑ups.
- Emotional support from a mental health counselor or a trusted friend who understands the anxiety that comes with unpredictable symptoms.
- Peer support through a patient advocacy group or an online forum where people exchange real‑world tricks.
- Remote care via a telehealth platform that lets you chat with doctors without leaving the house.
- Local community resources such as a community center that hosts wellness workshops.
Finding the Right Resources
Start with a quick online search for "proctitis support" plus your city or ZIP code. You’ll often find a mix of national groups (like the Crohn’s & Colitis Foundation) and hyper‑local meetups posted on platforms such as Meetup.com. Don’t overlook disease‑specific sub‑forums on sites like Reddit’s r/IBD; they have dedicated threads for rectal inflammation.
For paid services, compare a few telehealth apps. Look at features like secure messaging, prescription handling, and whether they offer a dedicated IBD specialist. Many insurers now cover virtual visits for chronic bowel conditions, so check your plan’s benefits.
Building Your Personal Support Circle
Once you’ve identified resources, it’s time to turn them into a circle that works for you. Here’s a step‑by‑step routine:
- Write down the types of support you need (medical, dietary, emotional, practical).
- Reach out to at least one professional in each category. A quick email or phone call is enough to gauge responsiveness.
- Join one online forum and introduce yourself. Share a brief overview of your diagnosis and what you hope to learn.
- Attend a local meet‑up or community‑center workshop within the next month. Face‑to‑face interaction builds trust faster than text alone.
- Set a recurring reminder (weekly or bi‑weekly) to check in with each contact. Consistency keeps the network alive.
Remember, a support network is a two‑way street. Offer what you can-maybe a recipe that helped you, a reminder about a new medication, or simply a listening ear. Giving back strengthens the bond and makes others more inclined to help you when you need it.
Overcoming Common Roadblocks
Even with the best intentions, challenges pop up:
- Stigma. Talking about bowel issues still feels taboo for many. Counter this by framing the conversation around overall well‑being rather than just symptoms.
- Privacy concerns. Use pseudonyms on public forums and choose platforms with strong data encryption. For in‑person groups, ask the facilitator about confidentiality policies.
- Burnout. Managing appointments, diet logs, and emotional check‑ins can feel overwhelming. Schedule “reset” days where you disengage from all health‑related communication.
When a hurdle feels too big, lean on a mental‑health counselor. Cognitive‑behavioral techniques can reframe anxiety about flare‑ups and help you set realistic expectations for your support circle.
Choosing the Right Peer Platform: A Quick Comparison
| Support Type | Meeting Frequency | Cost | Accessibility | Level of Anonymity |
|---|---|---|---|---|
| In‑person support group | Weekly or bi‑weekly | Free‑or‑low fee (venue cost) | Requires travel to a local venue | Low - you use your real name |
| Online forum (e.g., Reddit) | Anytime, self‑paced | Free | Internet access only | High - usernames can be pseudonymous |
| Peer‑to‑peer app (e.g., HealthUnlocked) | Daily notifications | Free with optional premium | Mobile app, works on the go | Medium - profile can be limited |
Maintaining Momentum Over Time
After the first few weeks, the novelty can wear off. Keep the energy up by:
- Rotating the role of meeting facilitator among group members.
- Setting a monthly “topic‑of‑the‑month” (e.g., low‑FODMAP recipes, stress‑reduction techniques).
- Celebrating small wins-like a week with fewer bathroom trips or a successful diet tweak.
- Periodically revisiting your support‑needs checklist to add or remove contacts.
When you notice a drop in engagement, reach out individually. A quick text asking, “Hey, how’s your week going?” can reignite participation.
Frequently Asked Questions
Can I join a support group if I’m newly diagnosed?
Absolutely. Most groups welcome members at any stage because fresh perspectives help everyone understand the disease’s early challenges.
What should I look for in an online forum?
Prioritize active moderation, clear rules on privacy, and a high posting frequency. Forums with verified medical professionals participating add extra credibility.
Is telehealth covered by insurance for proctitis?
Many US insurers now include virtual visits for chronic gastrointestinal conditions. Check your policy’s “telehealth” clause or call the member services line for specifics.
How often should I meet with my gastroenterologist?
During stable periods, a quarterly check‑up is typical. If you experience frequent flare‑ups, your doctor may recommend monthly visits or urgent virtual appointments.
What are some simple diet changes that help?
Start with a low‑FODMAP diet, stay hydrated, and avoid spicy or high‑fiber foods that can irritate the rectal lining. A nutritionist can personalize the plan based on your tolerance.

Key Takeaways
- A dedicated support network lowers emergency visits and improves quality of life.
- Mix medical, nutritional, emotional, and peer support for a well‑rounded approach.
- Use both local in‑person groups and online platforms to maximize reach.
- Regular check‑ins and clear communication keep the network active.
- Address stigma, privacy, and burnout early to sustain long‑term support.


Life is a river, and support is the current that keeps us moving.
Alright folks, let’s break down why a solid support crew is the secret sauce for tackling proctitis.
First off, having someone to vent to reduces the stress hormones that can actually flare up your gut.
Stress releases cortisol, and cortisol is a known trigger for inflammatory bowel episodes, so the mental side matters as much as the meds.
Second, peer groups often share nuggets of practical advice like which low‑FODMAP snacks actually stay down without causing a midnight dash to the bathroom.
I’ve seen members swap recipes that replace problematic garlic and onions with ginger‑turmeric blends that soothe the lining.
Third, regular check‑ins force you to keep a symptom diary, which gives your gastroenterologist concrete data instead of vague descriptions.
When you bring numbers to the appointment, the doc can fine‑tune your medication faster and avoid unnecessary steroid bursts.
Fourth, feeling seen and heard cuts the isolation factor that makes many patients skip appointments out of embarrassment.
You’re far less likely to hide a flare when a buddy already knows the warning signs and can remind you to call the clinic.
Fifth, online forums let you scroll through archived threads at 2 am, so you’re never stuck Googling “why does my poop hurt” without context.
Sixth, telehealth platforms give you a quick text‑to‑doc line, so you don’t have to brave traffic when your symptoms suddenly spike.
Seventh, community workshops often bring in dietitians who can personalize the low‑FODMAP plan to your cultural food preferences.
Eighth, rotating the facilitator role keeps meetings fresh, because nobody wants the same voice drone on forever.
Ninth, celebrating tiny wins-like three days with no urgent bathroom trips-creates a positive feedback loop that fuels motivation.
Tenth, if burnout starts to creep in, set a ‘reset day’ where you mute all health notifications and just chill, because recovery is also mental.
Finally, remember that the network is a two‑way street: offering a tip or a listening ear makes others more eager to return the favor when you need it most.
Hey there I think the best thing is just to start small join a local group or even a Reddit thread and just say hi you’ll be surprised how friendly everyone is
I’ll be the first to admit that not every support group is a panacea, many operate more like echo chambers than problem‑solvers
Think of your support network as a training regimen; you schedule the workouts, track the progress, and rest when needed, and you’ll see steady improvement in both symptoms and confidence.
Oh, marvelous, another flawless prescription for success-because clearly the telehealth conglomerates have been plotting to replace our doctors with chatbots, haven’t they?
Honestly the US healthcare system already offers the best telehealth services, so why are we even discussin’ other options? It’s about time we appreciate what we have.
I completely understand how overwhelming this can feel, especially when symptoms flare unexpectedly, but please remember you’re not alone, many others share your journey, and together we can find strength.
The struggle is real and the pain is intense but we must rise above it!
I love that you’re opening up about your fears 🙏✨, but don’t forget to share your favorite comfort food recipes too 🍲😊, it helps the whole group feel connected.
A supportive circle can truly change the day‑to‑day experience.
You’ve got this! Every small step you take builds a stronger foundation, and the community is right there cheering you on.
As most of us already know, the key to a thriving support net lies in consistent communication and diversified expertise.
Totally agree!!! Let’s all start a weekly virtual coffee ☕️ meet up where we can swap tips, vent, and maybe even do a quick yoga stretch together!!!
Let’s get moving, folks! Set a reminder, call a friend, and take that first step toward a healthier, happier you!
From a philosophical standpoint, community support mirrors the concept of interdependence in nature; each individual’s well‑being contributes to the collective resilience of the group.
Honestly if you’re not speaking up about your condition you’re being selfish and it’s just not ok.
You should prioritize a gastroenterologist above all else; anything less is simply inadequate care.
Allow me to correct a common mistake: It is ‘proctitis patients’ not ‘proctitis patient’s’; proper apostrophe placement is essential for clarity.