Combining aspirin with other blood thinners might seem like a smart way to protect your heart - but it can put you at serious risk of dangerous bleeding. This isn’t just a theoretical concern. Real people in real situations are ending up in emergency rooms because of this mix. If you’re taking aspirin daily and your doctor added a blood thinner like warfarin, rivaroxaban, or apixaban, you need to understand exactly what’s happening in your body - and why the risks might outweigh the benefits.
How Aspirin and Blood Thinners Work Together (and Why That’s Dangerous)
Aspirin doesn’t work like most blood thinners. It’s not an anticoagulant - it’s an antiplatelet. That means it stops your platelets from clumping together to form clots. It does this by blocking an enzyme called cyclooxygenase-1, which reduces a substance called thromboxane A2. Less thromboxane means platelets can’t stick as easily. Simple enough.
But drugs like warfarin, rivaroxaban, dabigatran, and apixaban work differently. They target the clotting cascade - the chain reaction of proteins that turns blood from liquid to solid. These are called oral anticoagulants (OACs). When you take aspirin and an OAC together, you’re hitting clotting from two sides at once. Your body’s natural ability to stop bleeding gets seriously weakened.
This isn’t just adding two risks. It’s multiplying them. Studies show the chance of major bleeding nearly doubles when aspirin is combined with any OAC. And it’s not just one type of bleeding. The danger shows up in your stomach, brain, lungs, and even your urine.
Where the Bleeding Happens - And How Bad It Gets
Most people think of bleeding as a cut that won’t stop. But internal bleeding from this combo is silent and deadly. Here’s what the data says:
- Gastrointestinal bleeding: 2.24 times more likely. This can mean slow, unnoticed blood loss in your gut - leading to anemia, fatigue, or even black, tarry stools.
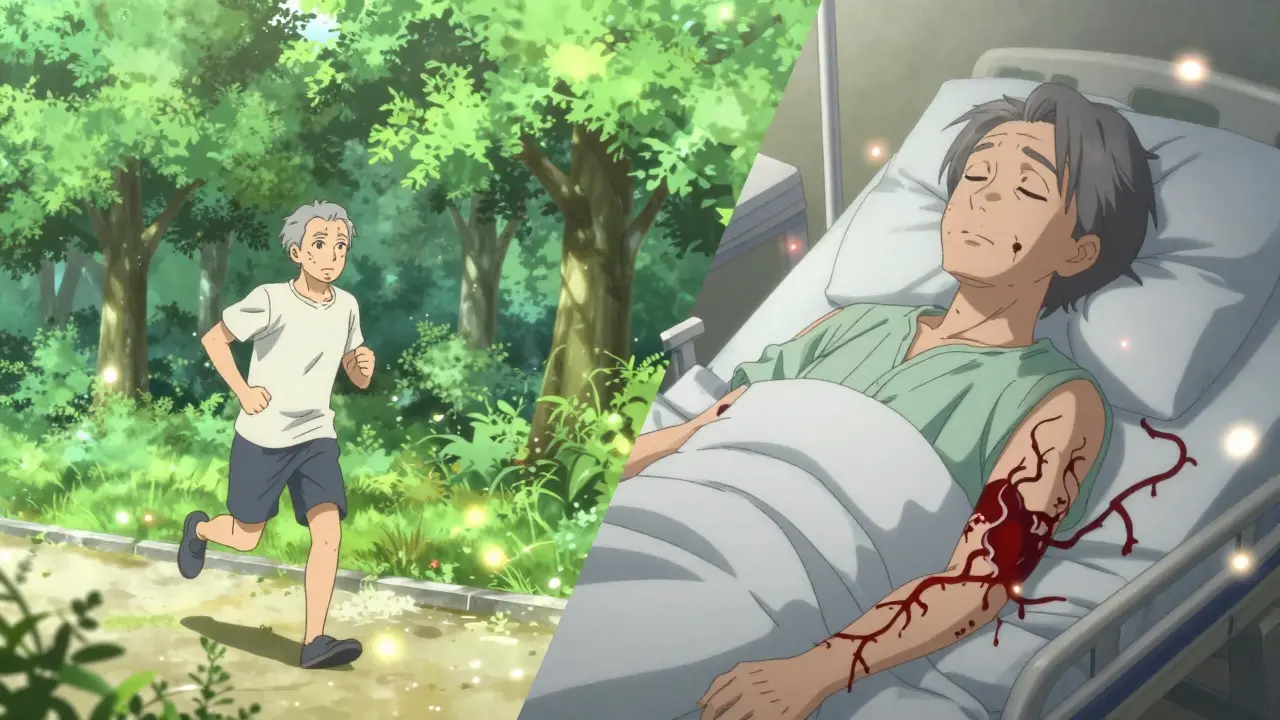
- Intracranial bleeding: 3.22 times more likely. A bleed in the brain is one of the most dangerous outcomes. The ASPREE trial, which followed nearly 20,000 healthy older adults, found daily aspirin increased the risk of traumatic brain bleeds by 38% compared to placebo.
- Pulmonary bleeding: 1.36 times higher. This can cause coughing up blood or sudden shortness of breath.
- Urinary tract bleeding: 1.57 times higher. Blood in the urine isn’t normal - and when it happens with aspirin and a blood thinner, it’s a red flag.
Anemia from hidden bleeding is nearly three times more common in people on both drugs. You might feel tired, dizzy, or short of breath - and not realize it’s because your body is slowly losing blood.
Not All Blood Thinners Are the Same
Some combinations are riskier than others. Among the newer anticoagulants (NOACs), rivaroxaban carries the highest bleeding risk when paired with aspirin, according to a 2024 meta-analysis of 24 studies. Warfarin, the older option, also increases bleeding risk - but it’s easier to monitor with regular blood tests.
And it’s not just prescription drugs. Over-the-counter painkillers like naproxen and diclofenac can make things worse. Naproxen with an OAC raises bleeding risk by 4.1 times. Diclofenac? 3.3 times. Even ibuprofen - something many people take for headaches - increases risk by almost 80%.
That’s why the FDA added boxed warnings to NSAID labels - the strongest warning they can give. It’s not just aspirin. It’s the whole group of drugs that affect platelets and clotting.
Who Should Avoid This Combo - And Who Might Still Need It
For healthy people over 60, daily aspirin for heart protection is no longer recommended. The National Institute on Aging says the risks - especially bleeding - outweigh any benefit. The U.S. Preventive Services Task Force updated its guidelines in 2022 to reflect this. Fewer people are taking aspirin for primary prevention now.
But if you’ve had a heart attack, stroke, or have a mechanical heart valve, the story changes. In those cases, the risk of another clot can be life-threatening. That’s when doctors might still prescribe aspirin with a blood thinner - but only after careful thought.
Experts like Dr. Søren Riis Petersen and Dr. Weinrauch agree: unless there’s a clear, strong reason, don’t mix them. If you have high blood pressure, kidney disease, a history of ulcers, or any bleeding disorder, the danger skyrockets.
What You Can Do to Stay Safe
If you’re on both aspirin and a blood thinner, don’t stop either without talking to your doctor. But do take these steps:
- Use an electric razor instead of a blade - even a small nick can bleed longer than expected.
- Switch to a soft-bristle toothbrush. Gum bleeding is common, but it shouldn’t be constant.
- Wear protective gear if you’re active - helmets, knee pads, even gloves when gardening.
- Take aspirin with food. It reduces stomach irritation and lowers the chance of GI bleeding.
- Know the warning signs: unusual bruising, blood in stool or urine, headaches that won’t go away, dizziness, or feeling faint.
Your doctor should be checking your hemoglobin levels regularly. If you’re on warfarin, you’re probably already getting INR tests. But even with NOACs, blood tests to check for anemia are important.
Tools like the HAS-BLED score help doctors measure your bleeding risk. It looks at things like high blood pressure, kidney or liver disease, stroke history, and whether you’re on multiple blood-thinning drugs. If your score is high, your doctor might reconsider the combination.

The Bigger Picture - Why This Is Still Common
Despite the risks, about 29 million Americans still take daily aspirin. Many do it out of habit - or because they heard it "helps the heart." The global anticoagulant market is growing fast, projected to hit $66.2 billion by 2029. More people are on NOACs than ever before.
But the science is clear: unless you have a specific, high-risk condition like a mechanical heart valve or recent stent placement, the combo is rarely worth it. Ongoing research is looking at genetic testing - like checking for CYP2C9 and VKORC1 variants - to better tailor warfarin doses. But for now, the safest approach is simple: use the fewest drugs possible.
Some doctors still prescribe aspirin with NOACs out of caution - but that’s changing. The 2024 American Journal of Health-System Pharmacy review recommends limiting this combo to only the most essential cases - and even then, with close monitoring.
When to Call Your Doctor Immediately
Don’t wait. If you notice any of these, get help right away:
- Bleeding that doesn’t stop after 10 minutes of pressure
- Dark, tarry, or bloody stools
- Red or pink urine
- Vomiting blood or material that looks like coffee grounds
- Sudden, severe headache, confusion, or vision changes
- Unexplained swelling, pain, or bruising - especially on the head or abdomen
These aren’t "wait and see" symptoms. They’re emergencies. Call your doctor or go to the ER. Tell them you’re taking aspirin and a blood thinner. That detail could save your life.
Can I take aspirin with warfarin?
Taking aspirin with warfarin increases your risk of serious bleeding, especially in the stomach and brain. This combination is only used in rare cases - like after a heart stent or with a mechanical heart valve. For most people, the risks outweigh the benefits. Always consult your doctor before combining them.
Is it safe to take aspirin with rivaroxaban or apixaban?
No, not without strong medical justification. Rivaroxaban has the highest bleeding risk when combined with aspirin among the newer blood thinners. Studies show a significant increase in major bleeding events - including fatal ones. Most guidelines now discourage this combo unless you have a specific, life-threatening clotting condition.
What should I do if I accidentally took ibuprofen with my blood thinner?
One dose of ibuprofen is unlikely to cause immediate bleeding, but it still increases your risk. Stop taking it and switch to acetaminophen (paracetamol) for pain relief - it doesn’t affect platelets. Tell your doctor about the interaction. If you notice unusual bruising, blood in stool, or dizziness, seek medical help right away.
Can I stop aspirin on my own if I’m on a blood thinner?
Never stop aspirin suddenly if your doctor prescribed it for a heart condition - like after a stent or heart attack. Stopping it can trigger a clot. But if you’re taking it for general prevention and are on a blood thinner, talk to your doctor. They may recommend stopping it safely. Never make this decision alone.
Are there safer alternatives to aspirin for heart protection?
For most people, the best way to protect your heart isn’t aspirin - it’s lifestyle. Regular exercise, a low-sodium diet, not smoking, and managing blood pressure and cholesterol are proven to reduce heart attack risk without bleeding side effects. If you have a high risk, your doctor may prescribe a different medication - like a statin - that doesn’t interfere with clotting.
Final Thoughts - Less Is Often More
Medicine has gotten better at preventing clots - but we’ve also learned that too many drugs can be just as dangerous as the condition we’re trying to treat. Aspirin isn’t harmless. Blood thinners aren’t harmless. Together, they create a perfect storm for bleeding.
If you’re on both, ask your doctor: "Is this combination still necessary?" If you’re not sure why you’re taking aspirin, find out. Many people take it out of habit, not because it’s helping them. The goal isn’t to take more pills - it’s to stay healthy with the fewest risks possible.


Aspirin with anticoagulants is a recipe for disaster unless you’re post-stent or have a mechanical valve. I’ve seen three patients bleed out from GI bleeds because their PCP just kept them on both ‘just in case.’ Don’t be one of them.
OMG I JUST REALIZED I’VE BEEN TAKING IBUPROFEN WITH APIXABAN FOR MY KNEE PAIN 😱 I’M SO SCARED RIGHT NOW. I’M GOING TO CALL MY DOCTOR RIGHT NOW. 💔🩸 #BleedingRisk #HealthWakeUpCall
You know, it’s funny how we’ve been conditioned to think more pills = better health. We’ve turned medicine into a buffet instead of a carefully balanced meal. Aspirin was once a miracle drug - now it’s just another habit we cling to because we’re afraid of being vulnerable to death. But the truth? Our bodies are smarter than our prescriptions. We don’t need to force them into compliance with chemical cocktails. Sometimes, silence - no pills, no noise - is the most healing thing we can do. The real question isn’t whether you should take aspirin with a blood thinner… it’s whether you should be taking anything at all.
I just lost my dad to a brain bleed last year. He was 72, took aspirin daily for ‘heart health’ since the 90s, and got prescribed rivaroxaban after a TIA. His doctor never told him the combo could kill him. He just said ‘it’s fine.’ He went to sleep one night and never woke up. No warning. No pain. Just… gone. I’ve been screaming into the void since then trying to make people understand - this isn’t theoretical. It’s real. And it’s happening to your neighbor, your cousin, your uncle. Please, if you’re on both - ask your doctor if it’s still necessary. Not ‘is it okay?’ - but ‘is it still needed?’
Let’s be clear: this isn’t a medical issue - it’s a systemic failure of the pharmaceutical-industrial complex. Big Pharma profits off polypharmacy. They market aspirin like it’s a vitamin, then slap on a boxed warning when the damage is done. Meanwhile, doctors are overworked, underpaid, and incentivized to prescribe, not question. We’re not patients - we’re revenue streams. And now we’re expected to read 5,000-word blog posts to avoid dying from a drug combo that shouldn’t have been approved in the first place. The system is broken. And until we stop treating medicine like a product, people will keep dying because someone thought ‘two anticoagulants can’t hurt.’
Wow. Someone actually wrote a responsible post about aspirin. Shocking. I’m assuming you’re not a rep for Bayer or a cardiologist on a speaking tour. Either way, congrats on not being an idiot. Most people still think aspirin is a daily multivitamin. Spoiler: it’s not. It’s a blunt instrument. And combining it with a NOAC? That’s like putting a flamethrower on a candle. You’re not protecting your heart - you’re just making sure your next funeral has a bigger bloodstain on the coffin.
I get why people do this - fear. Fear of heart attack, fear of stroke, fear of dying. But fear doesn’t make good medicine. I’ve been on apixaban for AFib for 4 years. My doc added aspirin after my stent - but we re-evaluated it after 6 months. My HAS-BLED score was 4. We dropped aspirin. No clots. No bleeds. Just peace of mind. The truth? Most people don’t need it. And if you’re over 60 and healthy? You definitely don’t. It’s not about being brave - it’s about being smart.
hey i was on warfarin and aspirin for like 2 years after my heart attack and my INR was always wild. my doc finally said ‘stop the aspirin’ and my numbers stabilized. i thought i was being extra safe but turns out i was just being dumb. now i take a statin and walk 5 miles a day. no aspirin. no drama. just feelin’ good. ps: ibuprofen is a trap. use tylenol if you gotta.
There’s a quiet epidemic here - people taking meds because they’ve always taken them, not because they need them. We’ve lost the art of deprescribing. We’re taught to add, never to subtract. But sometimes, the most powerful medical decision isn’t starting a drug - it’s stopping one. If you’re on aspirin and an anticoagulant, ask yourself: ‘If I hadn’t started this, would I still be taking it?’ If the answer’s no - you’ve already answered your question. Your body doesn’t need more chemicals. It needs clarity. And sometimes, that means doing less.
I’m 68 and I’ve been on aspirin since 2010. My doctor never said ‘stop.’ So I didn’t. Then my sister had a GI bleed and nearly died. I asked my doc ‘is this still worth it?’ He said ‘probably not.’ I stopped. No heart attack. No stroke. Just… me. Alive. And not bleeding. Sometimes the best treatment is just… stopping.
Let’s not pretend this is about health. This is about liability. Doctors prescribe this combo because if you have a clot, they’re blamed. If you bleed? Well… you were ‘on multiple anticoagulants.’ It’s not medicine - it’s insurance. And you? You’re the cost center. Congratulations. You’re the human sacrifice in the altar of defensive medicine. Wake up. Your life isn’t a risk-management spreadsheet.
My dad died from a brain bleed at 71. He took aspirin and Eliquis. The ER doc said ‘this is exactly what we warn about.’ I didn’t know. No one told me. Now I’m the one telling people. Don’t wait for a hospital visit to learn this. Ask your doctor now. If they hesitate - that’s your answer.